4.2 Epithelial Tissue
Learning Objectives
Describe the structural characteristics of the various epithelial tissues and how these characteristics enable their functions.
By the end of this section, you will be able to:
- Explain the general structure and function of epithelial tissue
- Distinguish between tight junctions, anchoring junctions, and gap junctions
- Distinguish between simple epithelia and stratified epithelia, as well as between squamous, cuboidal, and columnar epithelia
- Describe the structure and function of endocrine and exocrine glands
Epithelial tissue primarily appears as large sheets of cells covering all surfaces of the body exposed to the external environment and lining internal body cavities. In addition, epithelial tissue is responsible for forming a majority of glandular tissue found in the human body.
Epithelial tissue is derived from all three major embryonic layers. The epithelial tissue composing cutaneous membranes develops from the ectoderm. Epithelial tissue composing a majority of the mucous membranes originate in the endoderm. Epithelial tissue that lines vessels and open spaces within the body are derived from mesoderm. Of particular note, epithelial tissue that lines vessels in the lymphatic and cardiovascular systems is called endothelium whereas epithelial tissue that forms the serous membranes lining the true cavities is called mesothelium.
Regardless of its location and function, all epithelial tissue shares important structural features. First, epithelial tissue is highly cellular, with little or no extracellular material present between cells. Second, adjoining cells form specialized intercellular connections called cell junctions. Third, epithelial cells exhibit polarity with differences in structure and function between the exposed, or apical, facing cell surface and the basal surface closest to the underlying tissue. Fourth, epithelial tissues are avascular; nutrients must enter the tissue by diffusion or absorption from underlying tissues or the surface. Last, epithelial tissue is capable of rapidly replacing damaged and dead cells, necessary with respect to the harsh environment this tissue encounters.
Epithelial Tissue Function:
Epithelial tissues provide the body’s first line of protection from physical, chemical, and biological damage. The cells of an epithelium act as gatekeepers of the body, controlling permeability by allowing selective transfer of materials across its surface. All substances that enter the body must cross an epithelium.
Many epithelial cells are capable of secreting mucous and other specific chemical compounds onto their apical surfaces. For example, the epithelium of the small intestine releases digestive enzymes and cells lining the respiratory tract secrete mucous that traps incoming microorganisms and particles.
The Epithelial Cell
Epithelial cells are typically characterized by unequal distribution of organelles and membrane-bound proteins between their apical and basal surfaces. Structures found on some epithelial cells are an adaptation to specific functions. For example, cilia are extensions of the apical cell membrane that are supported by microtubules. These extensions beat in unison, allowing for the movement of fluids and particles along the surface. Such ciliated epithelia line the ventricles of the brain where it helps circulate cerebrospinal fluid and line the respirtatory system where it helps sweep particles of dust and pathogens up and out of the respiratory tract.
Epithelial cells in close contact with underlying connective tissues secrete glycoproteins and collagen from their basal surface which forms the basal lamina. The basal lamina interacts with the reticular lamina secreted by the underlying connective tissue, forming a basement membrane that helps anchor the layers together.
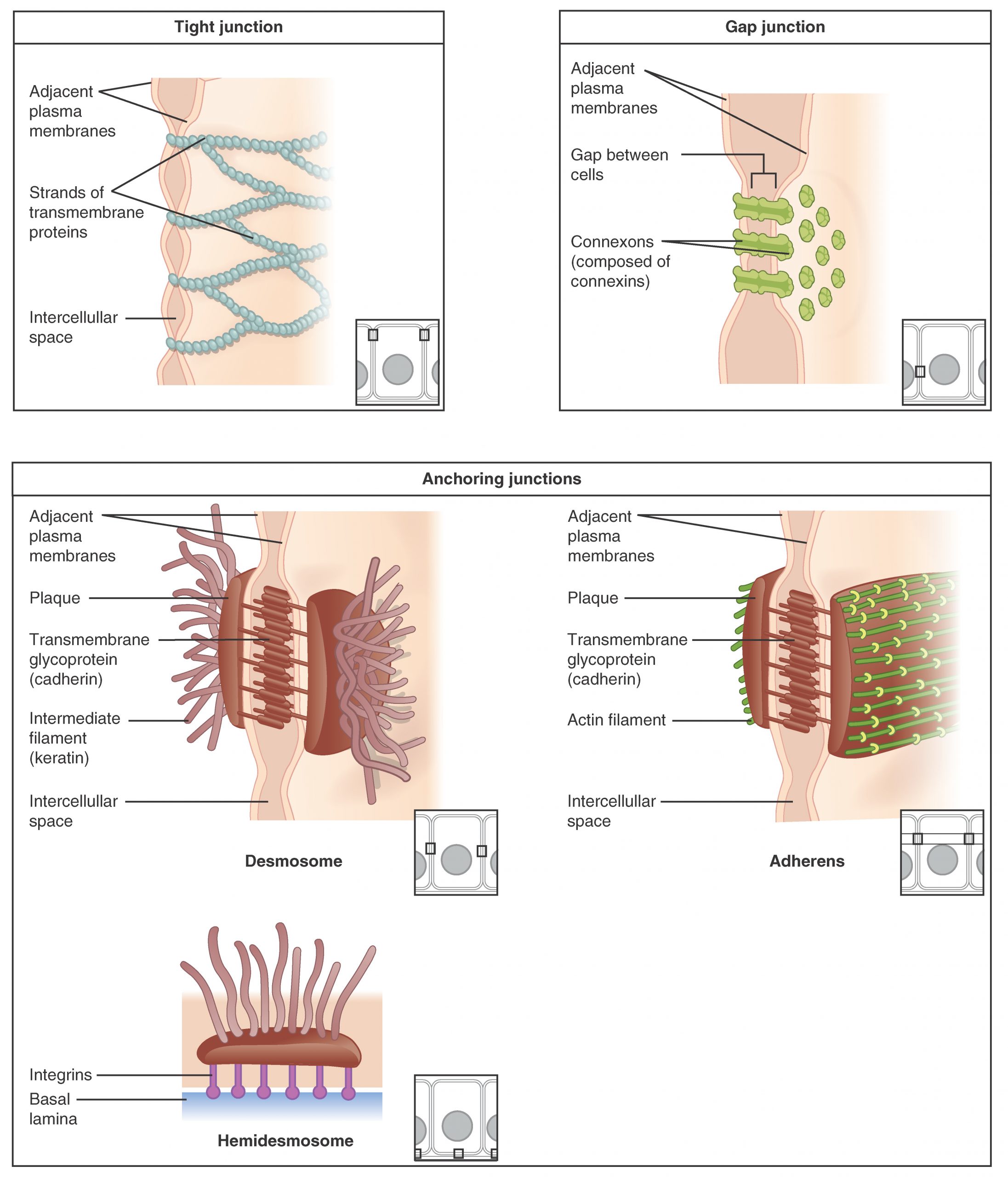
Cells of epithelia are closely connected with limited extracellular material present. Three basic types of connections may be present: tight junctions, anchoring junctions, and gap junctions (Figure 4.2.1).
Types of Cell Junctions
Epithelial cells are held close together by cell junctions. The three basic types of cell-to-cell junctions are tight junctions, gap junctions, and anchoring junctions.
A Tight junction restricts the movement of fluids between adjacent cells due to the presence of integral proteins that fuse together to form a firm seal. Tight junctions are observed in the epithelium of the urinary bladder, preventing the escape of fluids comprising the urine.
An anchoring junction provides a strong yet flexible connection between epithelial cells. There are three types of anchoring junctions: desmosomes, hemidesmosomes, and adherens. Desmosomes hold neighboring cells together by way of cadherin molecules which are embedded in protein plates in the cell membranes and link together between the adjacent cells. Hemidesmosomes, which look like half a desmosome, link cells to components in the extracellular matrix, such as the basal lamina. While similar in appearance to desmosomes, hemidesmosomes use adhesion proteins called integrins rather than cadherins. Adherens use either cadherins or integrins depending on whether they are linking to other cells or matrix. These junctions are characterized by the presence of the contractile protein actin located on the cytoplasmic surface of the cell membrane. These junctions influence the shape and folding of the epithelial tissue.
In contrast with the tight and anchoring junctions, a gap junction forms an intercellular passageway between the membranes of adjacent cells to facilitate the movement of small molecules and ions between cells. These junctions thus allow electrical and metabolic coupling of adjacent cells.
Classification of Epithelial Tissues
Epithelial tissues are classified according to the shape of the cells composing the tissue and by the number of cell layers present in the tissue.(Figure 4.2.2) Cell shapes are classified as being either squamous (flattened and thin), cuboidal (boxy, as wide as it is tall), or columnar (rectangular, taller than it is wide). Similarly, cells in the tissue can be arranged in a single layer, which is called simple epithelium, or more than one layer, which is called stratified epithelium. Pseudostratified (pseudo- = “false”) describes an epithelial tissue with a single layer of irregularly shaped cells that give the appearance of more than one layer. Transitional describes a form of specialized stratified epithelium in which the shape of the cells, and the number of layers present, can vary depending on the degree of stretch within a tissue.
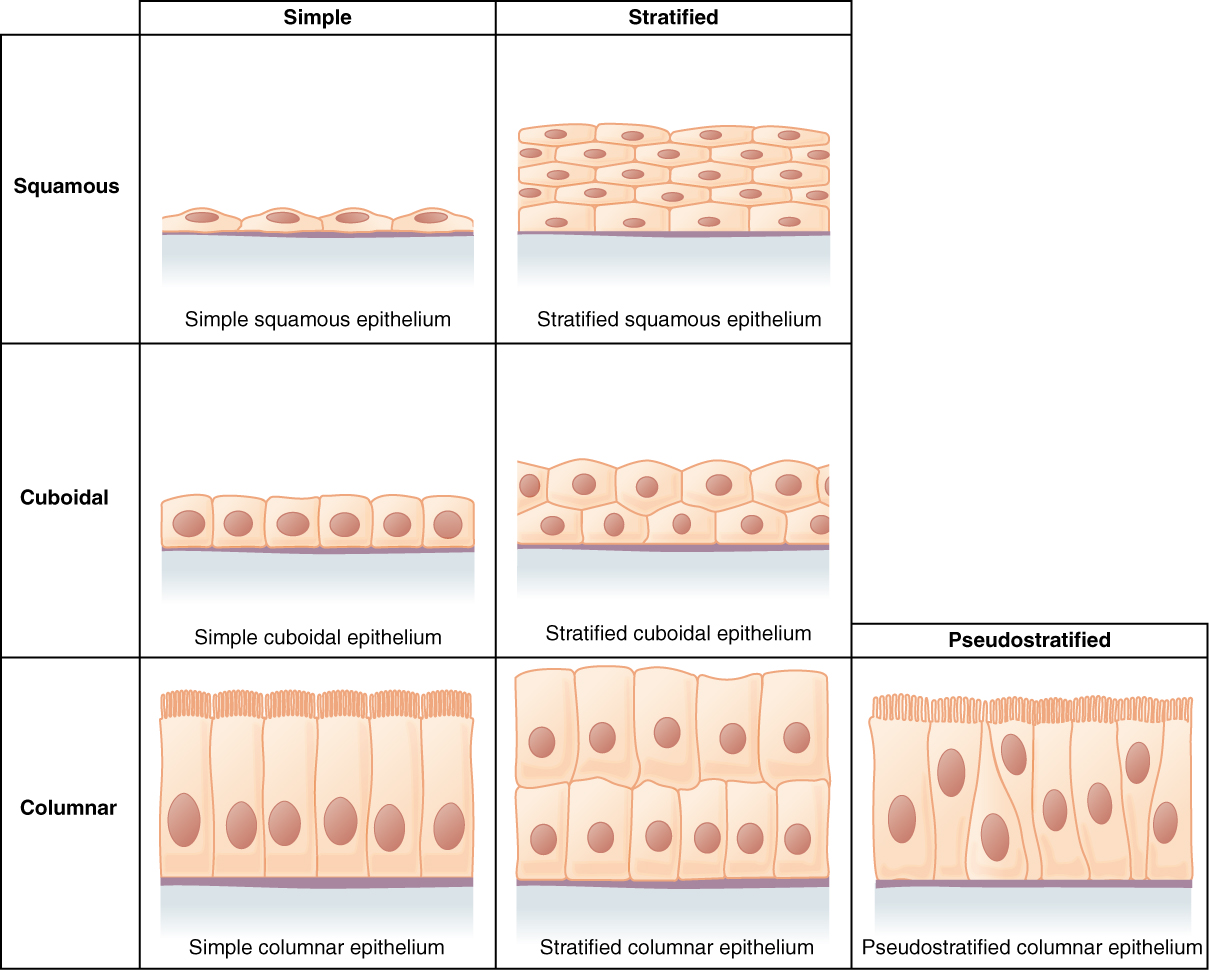
Epithelial tissue is classified based on the shape of the cells present and the number of cell layers present. Figure 4.2.2 summarizes the different categories of epithelial cell tissue cells.
External Website
Summary of Epithelial Tissue Cells
Watch this video to find out more about the anatomy of epithelial tissues. Where in the body would one find non-keratinizing stratified squamous epithelium?
Simple Epithelium
The cells in a simple squamous epithelium have the appearance of thin scales. The nuclei of squamous cells tend to appear flat, horizontal, and elliptical, mirroring the form of the cell. Simple squamous epithelium, because of the thinness of the cells, is present where rapid passage of chemical compounds is necessary such as the lining of capillaries and the small air sacs of the lung. This epithelial type is also found composing the mesothelium which secretes serous fluid to lubricate the internal body cavities.
In simple cuboidal epithelium, the nucleus of the box-like cells appears round and is generally located near the center of the cell. These epithelia are involved in the secretion and absorptions of molecules requiring active transport. Simple cuboidal epithelia are observed in the lining of the kidney tubules and in the ducts of glands.
In simple columnar epithelium, the nucleus of the tall column-like cells tends to be elongated and located in the basal end of the cells. Like the cuboidal epithelia, this epithelium is active in the absorption and secretion of molecules using active transport. Simple columnar epithelium forms a majority of the digestive tract and some parts of the female reproductive tract. Ciliated columnar epithelium is composed of simple columnar epithelial cells with cilia on their apical surfaces. These epithelial cells are found in the lining of the fallopian tubes where the assist in the passage of the egg, and parts of the respiratory system, where the beating of the cilia helps remove particulate matter.
Pseudostratified columnar epithelium is a type of epithelium that appears to be stratified but instead consists of a single layer of irregularly shaped and differently sized columnar cells. In pseudostratified epithelium, nuclei of neighboring cells appear at different levels rather than clustered in the basal end. The arrangement gives the appearance of stratification, but in fact, all the cells are in contact with the basal lamina, although some do not reach the apical surface. Pseudostratified columnar epithelium is found in the respiratory tract, where some of these cells have cilia.
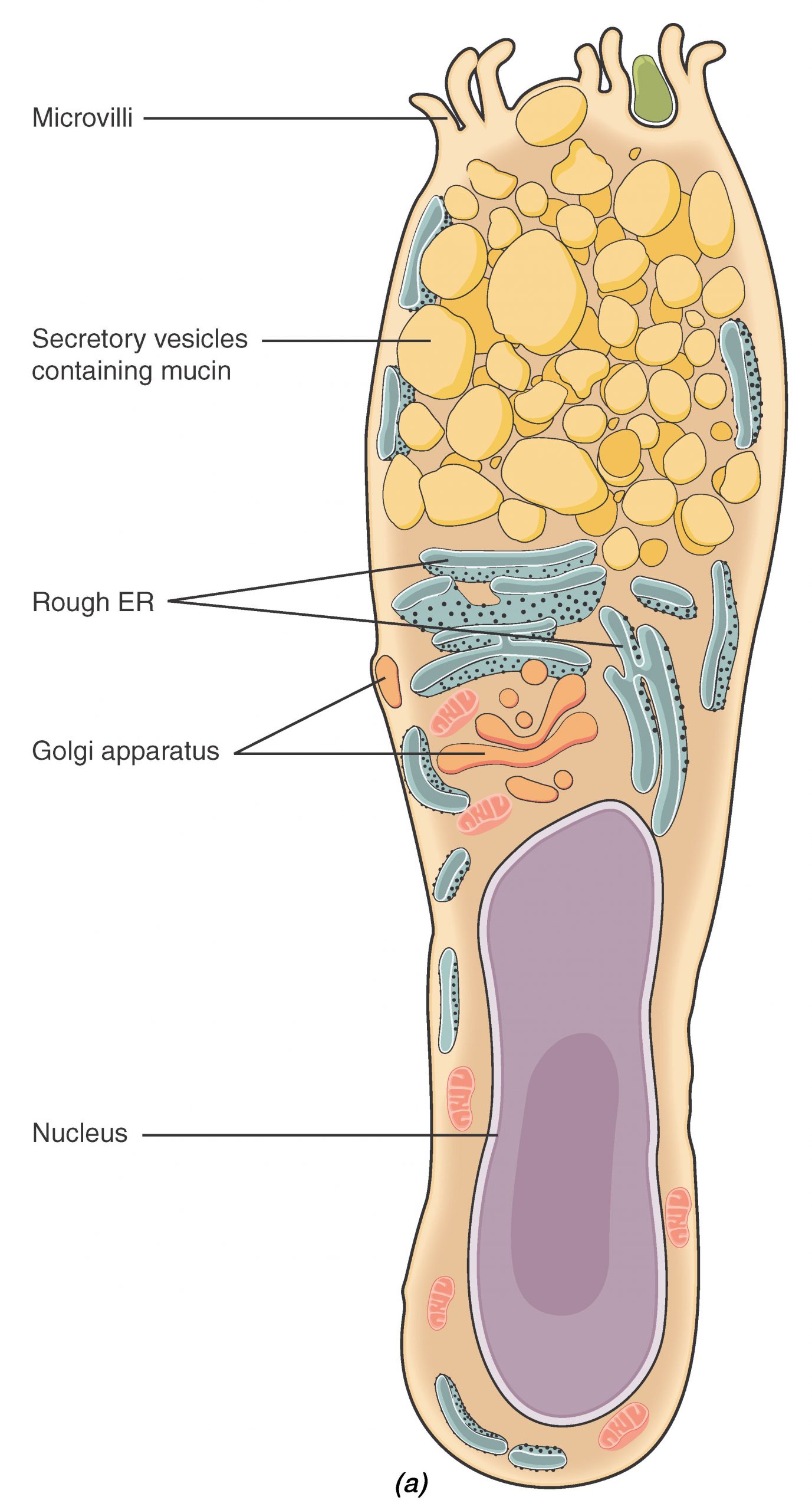
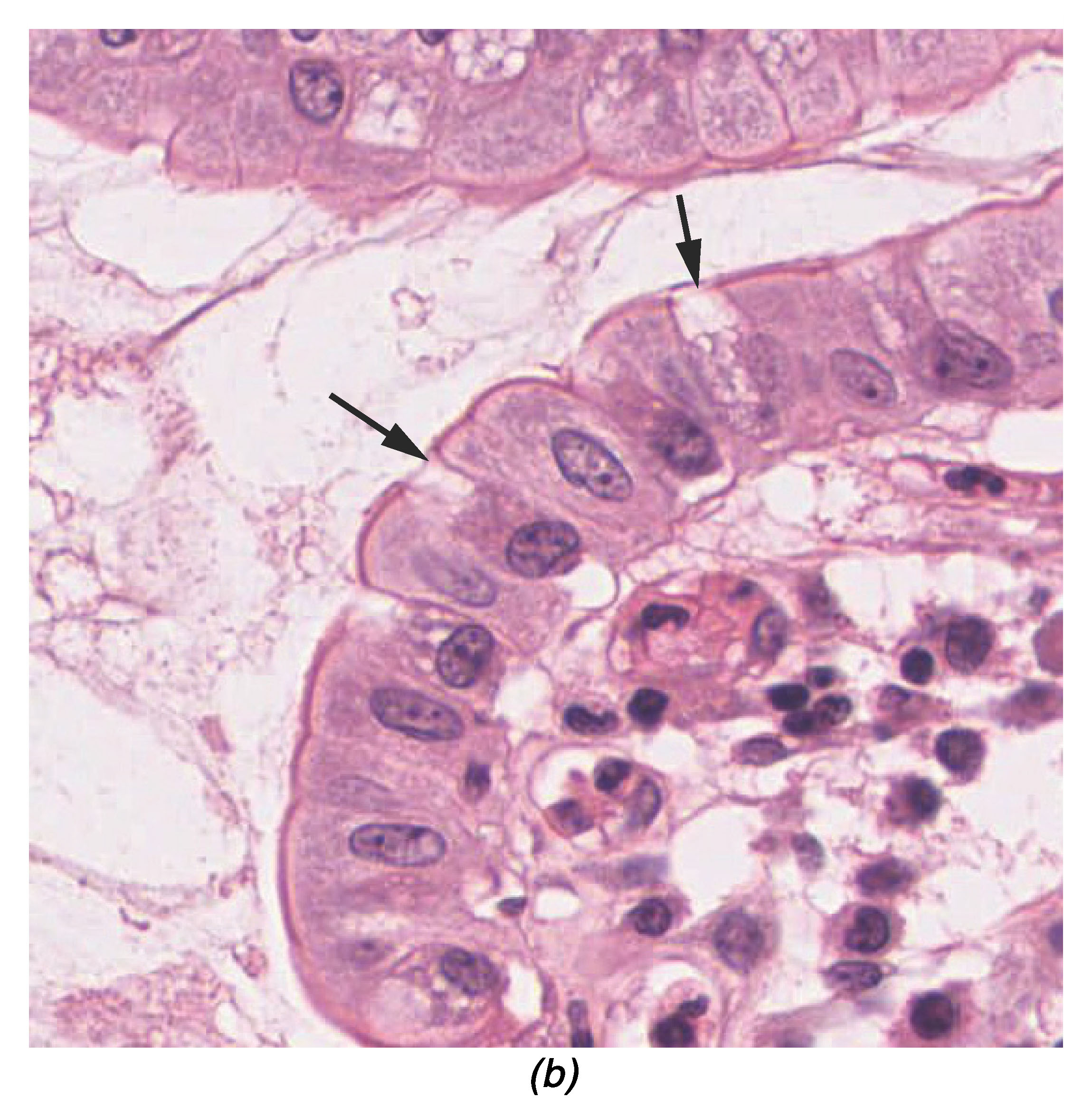
Both simple and pseudostratified columnar epithelia are heterogeneous epithelia because they include additional types of cells interspersed among the epithelial cells. For example, a goblet cell is a mucous-secreting unicellular gland interspersed between the columnar epithelial cells of a mucous membrane (Figure 4.2.3).
External Website

View the University of Michigan WebScope at http://virtualslides.med.umich.edu/Histology/Digestive%20System/Intestines/169_HISTO_40X.svs/view.apml to explore the tissue sample in greater detail.
Stratified Epithelium
A stratified epithelium consists of multiple stacked layers of cells. This epithelium protects against physical and chemical damage. The stratified epithelium is named by the shape of the most apical layer of cells, closest to the free space.
Stratified squamous epithelium is the most common type of stratified epithelium in the human body. The apical cells appear squamous, whereas the basal layer contains either columnar or cuboidal cells. The top layer may be covered with dead cells containing keratin. The skin is an example of a keratinized, stratified squamous epithelium. Alternatively, the lining of the oral cavity is an example of an unkeratinized, stratified squamous epithelium. Stratified cuboidal epithelium and stratified columnar epithelium can also be found in certain glands and ducts, but are relatively rare in the human body.
Another kind of stratified epithelium is transitional epithelium, so-called because of the gradual changes in the shapes and layering of the cells as the epithelium lining the expanding hollow organ is stretched. Transitional epithelium is found only in the urinary system, specifically the ureters and urinary bladder. When the bladder is empty, this epithelium is convoluted and has cuboidal-shaped apical cells with convex, umbrella shaped, surfaces. As the bladder fills with urine, this epithelium loses its convolutions and the apical cells transition in appearance from cuboidal to squamous. It appears thicker and more multi-layered when the bladder is empty, and more stretched out and less stratified when the bladder is full and distended.
Glandular Epithelium
A gland is a structure made up of one or more cells modified to synthesize and secrete chemical substances. Most glands consist of groups of epithelial cells. A gland can be classified as an endocrine gland, a ductless gland that releases secretions directly into surrounding tissues and fluids (endo- = “inside”), or an exocrine gland whose secretions leave through a duct that opens to the external environment (exo- = “outside”).
Endocrine Glands
The secretions of endocrine glands are called hormones. Hormones are released into the interstitial fluid, diffuse into the bloodstream, and are delivered to cells that have receptors to bind the hormones. The endocrine system a major communication system coordinating the regulation and integration of body responses. These glands will be discussed in much greater detail in a later chapter.
Exocrine Glands
Exocrine glands release their contents through a duct or duct system that ultimately leads to the external environment. Mucous, sweat, saliva, and breast milk are all examples of secretions released by exocrine glands.
Glandular Structure
Exocrine glands are classified as either unicellular or multicellular. Unicellular glands are individual cells which are scattered throughout an epithelial lining. Goblet cells are an example of a unicellular gland type found extensively in the mucous membranes of the small and large intestine.
Multicellular exocrine glands are composed of two or more cells which either secrete their contents directly into an inner body cavity (e.g., serous glands), or release their contents into a duct. If there is a single duct carrying the contents to the external environment then the gland is referred to as a simple gland. Multicellular glands that have ducts divided into one or more branches is called a compound gland (Figure 4.2.4). In addition to the number of ducts present, multicellular glands are also classified based on the shape of the secretory portion of the gland. Tubular glands have enlongated secretory regions (similar to a test tube in shape) while alveolar (acinar) glands have a secretory region that is spherical in shape. Combinations of the two secretory regions are known as tubuloalveolar (tubuloacinar) glands.
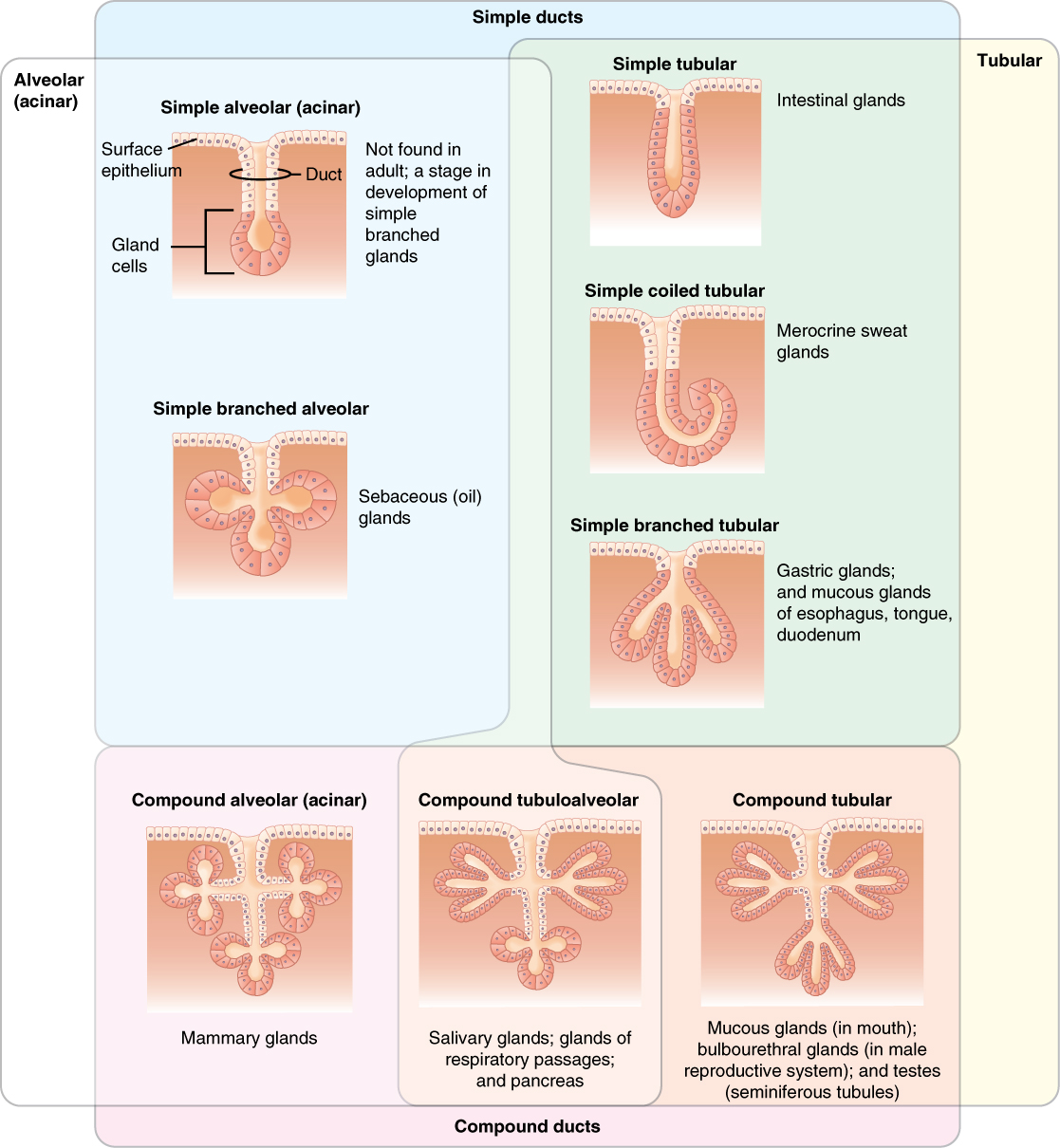
Exocrine glands are classified by the arrangement of ducts emptying the gland and the shape of the secretory region.
Methods and Types of Secretion
In addition to the glandular structure, exocrine glands can be classified by their mode of secretion and the nature of the substances released (Figure 4.2.5). Merocrine secretion is the most common type of exocrine secretion. The secretions are enclosed in vesicles that move to the apical surface of the cell where the contents are released by exocytosis. For example, saliva containing the glycoprotein mucin is a merocrine secretion. The glands that produce and secrete sweat are another example of merocrine secretion.
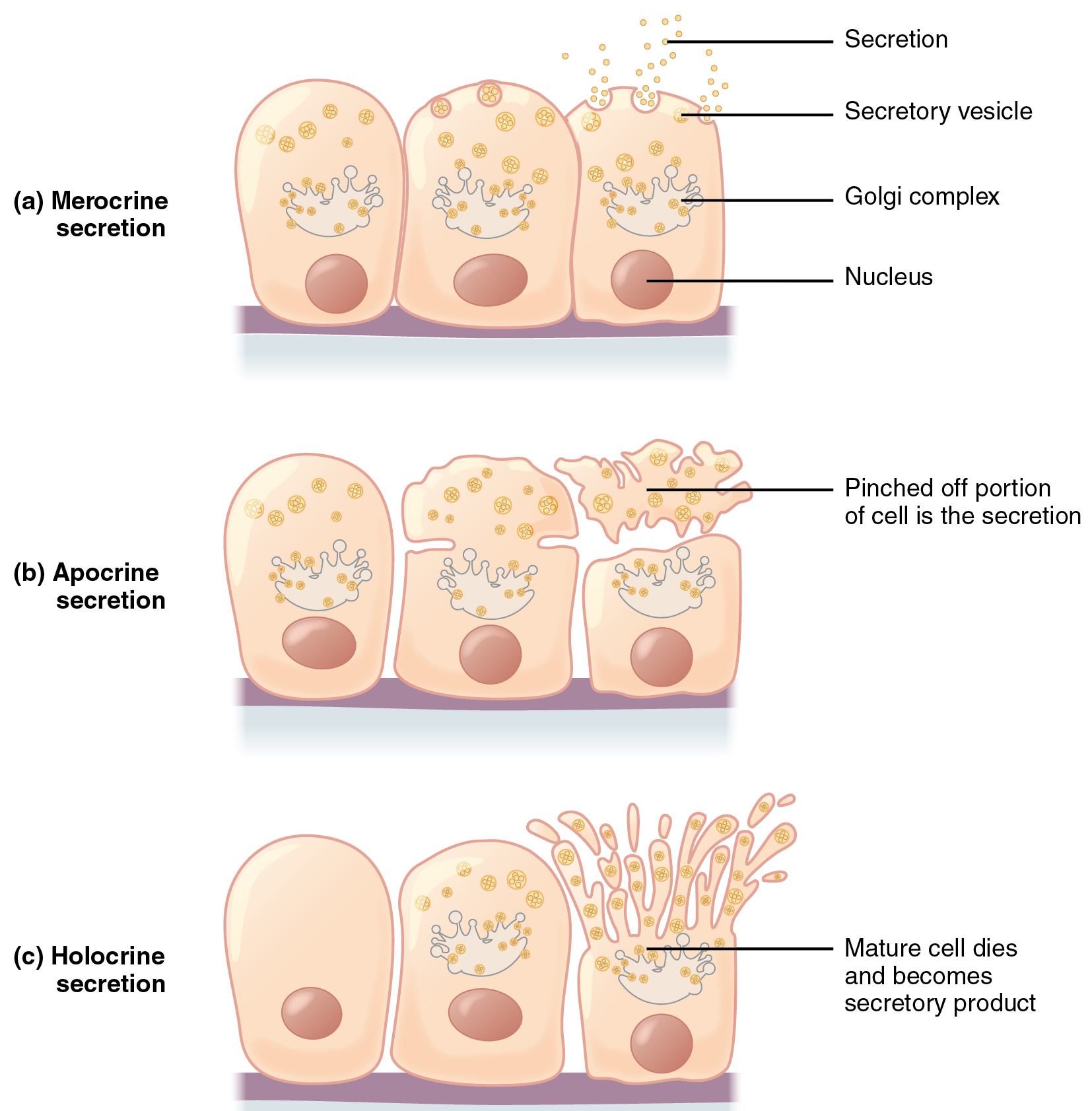
Apocrine secretion occurs when secretions accumulate near the apical portion of a secretory cell. That portion of the cell and its secretory contents pinch off from the cell and are released. The sweat glands of the armpit are classified as apocrine glands. Like merocrine glands, apocrine glands continue to produce and secrete their contents with little damage caused to the cell because the nucleus and golgi regions remain intact after the secretory event.
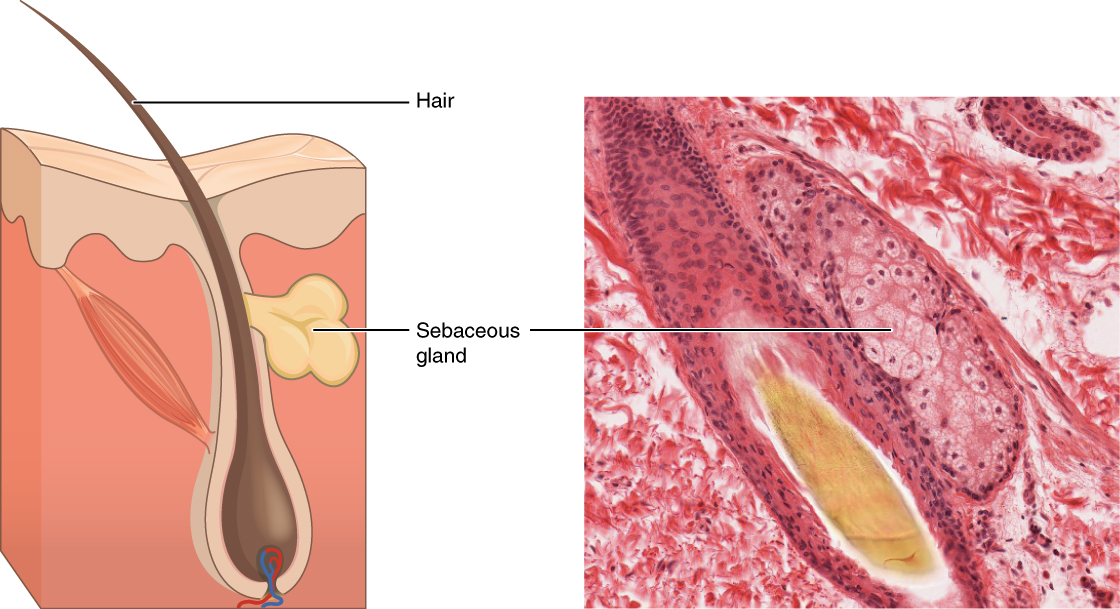
In contrast, the process of holocrine secretion involves the rupture and destruction of the entire gland cell. The cell accumulates its secretory products and releases them only when the cell bursts. New gland cells differentiate from cells in the surrounding tissue to replace those lost by secretion. The sebaceous glands that produce the oils on the skin and hair are an example of a holocrine glands (Figure 4.2.6).
Glands are also named based on the products they produce. A serous gland produces watery, blood-plasma-like secretions rich in enzymes, whereas a mucous gland releases a more viscous product rich in the glycoprotein mucin. Both serous and mucous secretions are common in the salivary glands of the digestive system. Such glands releasing both serous and mucous secretions are often referred to as seromucous glands.
Chapter Review
In epithelial tissue, cells are closely packed with little or no extracellular matrix except for the basal lamina that separates the epithelium from underlying tissue. The main functions of epithelia are protection from the environment, coverage, secretion and excretion, absorption, and filtration. Cells are bound together by tight junctions that form an impermeable barrier. They can also be connected by gap junctions, which allow free exchange of soluble molecules between cells, and anchoring junctions, which attach cell to cell or cell to matrix. The different types of epithelial tissues are characterized by their cellular shapes and arrangements: squamous, cuboidal, or columnar epithelia. Single cell layers form simple epithelia, whereas stacked cells form stratified epithelia. Very few capillaries penetrate these tissues.
Glands are secretory tissues and organs that are derived from epithelial tissues. Exocrine glands release their products through ducts. Endocrine glands secrete hormones directly into the interstitial fluid and blood stream. Glands are classified both according to the type of secretion and by their structure. Merocrine glands secrete products as they are synthesized. Apocrine glands release secretions by pinching off the apical portion of the cell, whereas holocrine gland cells store their secretions until they rupture and release their contents. In this case, the cell becomes part of the secretion.
Interactive Link Questions
Watch this video to find out more about the anatomy of epithelial tissues. Where in the body would one find non-keratinizing stratified squamous epithelium?
The inside of the mouth, esophagus, vaginal canal, and anus.
Review Questions
Critical Thinking Questions
The structure of a tissue usually is optimized for its function. Describe how the structure of individual cells and tissue arrangement of the intestine lining matches its main function, to absorb nutrients.
Columnar epithelia, which form the lining of the digestive tract, can be either simple or stratified. The cells are long and narrow. The nucleus is elongated and located on the basal side of the cell. Ciliated columnar epithelium is composed of simple columnar epithelial cells that display cilia on their apical surfaces.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.

