21.6 Diseases Associated with Depressed or Overactive Immune Responses
Learning Objectives
By the end of this section, you will be able to:
- Discuss inherited and acquired immunodeficiencies
- Explain the four types of hypersensitivity and how they differ
- Give an example of how autoimmune disease breaks tolerance
This section is about how the immune system goes wrong. When it goes haywire, and becomes too weak or too strong, it leads to a state of disease. The factors that maintain immunological homeostasis are complex and incompletely understood.
Immunodeficiencies
As you have seen, the immune system is quite complex. It has many pathways using many cell types and signals. Because it is so complex, there are many ways for it to go wrong. Inherited immunodeficiencies arise from gene mutations that affect specific components of the immune response. There are also acquired immunodeficiencies with potentially devastating effects on the immune system, such as HIV.
Inherited Immunodeficiencies
A list of all inherited immunodeficiencies is well beyond the scope of this book. The list is almost as long as the list of cells, proteins, and signaling molecules of the immune system itself. Some deficiencies, such as those for complement, cause only a higher susceptibility to some Gram-negative bacteria. Others are more severe in their consequences. Certainly, the most serious of the inherited immunodeficiencies is severe combined immunodeficiency disease (SCID). This disease is complex because it is caused by many different genetic defects. What groups them together is the fact that both the B cell and T cell arms of the adaptive immune response are affected.
Children with this disease usually die of opportunistic infections within their first year of life unless they receive a bone marrow transplant. Such a procedure had not yet been perfected for David Vetter, the “boy in the bubble,” who was treated for SCID by having to live almost his entire life in a sterile plastic cocoon for the 12 years before his death from infection in 1984. One of the features that make bone marrow transplants work as well as they do is the proliferative capability of hematopoietic stem cells of the bone marrow. Only a small amount of bone marrow from a healthy donor is given intravenously to the recipient. It finds its own way to the bone where it populates it, eventually reconstituting the patient’s immune system, which is usually destroyed beforehand by treatment with radiation or chemotherapeutic drugs.
New treatments for SCID using gene therapy, inserting nondefective genes into cells taken from the patient and giving them back, have the advantage of not needing the tissue match required for standard transplants. Although not a standard treatment, this approach holds promise, especially for those in whom standard bone marrow transplantation has failed.
Human Immunodeficiency Virus/AIDS
Although many viruses cause suppression of the immune system, only one wipes it out completely, and that is the previously mentioned HIV. It is worth discussing the biology of this virus, which can lead to the well-known AIDS, so that its full effects on the immune system can be understood. The virus is transmitted through semen, vaginal fluids, and blood, and can be caught by risky sexual behaviors and the sharing of needles by intravenous drug users. There are sometimes, but not always, flu-like symptoms in the first 1 to 2 weeks after infection. This is later followed by seroconversion. The anti-HIV antibodies formed during seroconversion are the basis for most initial HIV screening done in the United States. Because seroconversion takes different lengths of time in different individuals, multiple AIDS tests are given months apart to confirm or eliminate the possibility of infection.
After seroconversion, the amount of virus circulating in the blood drops and stays at a low level for several years. During this time, the levels of CD4+ cells, especially helper T cells, decline steadily, until at some point, the immune response is so weak that opportunistic disease and eventually death result. CD4 is the receptor that HIV uses to get inside T cells and reproduce. Given that CD4+ helper T cells play an important role in other in T cell immune responses and antibody responses, it should be no surprise that both types of immune responses are eventually seriously compromised.
Treatment for the disease consists of drugs that target virally encoded proteins that are necessary for viral replication but are absent from normal human cells. By targeting the virus itself and sparing the cells, this approach has been successful in significantly prolonging the lives of HIV-positive individuals. On the other hand, an HIV vaccine has been 30 years in development and is still years away. Because the virus mutates rapidly to evade the immune system, scientists have been looking for parts of the virus that do not change and thus would be good targets for a vaccine candidate.
Hypersensitivities
The word “hypersensitivity” simply means sensitive beyond normal levels of activation. Allergies and inflammatory responses to nonpathogenic environmental substances have been observed since the dawn of history. Hypersensitivity is a medical term describing symptoms that are now known to be caused by unrelated mechanisms of immunity. Still, it is useful for this discussion to use the four types of hypersensitivities as a guide to understand these mechanisms (Figure 21.6.1).
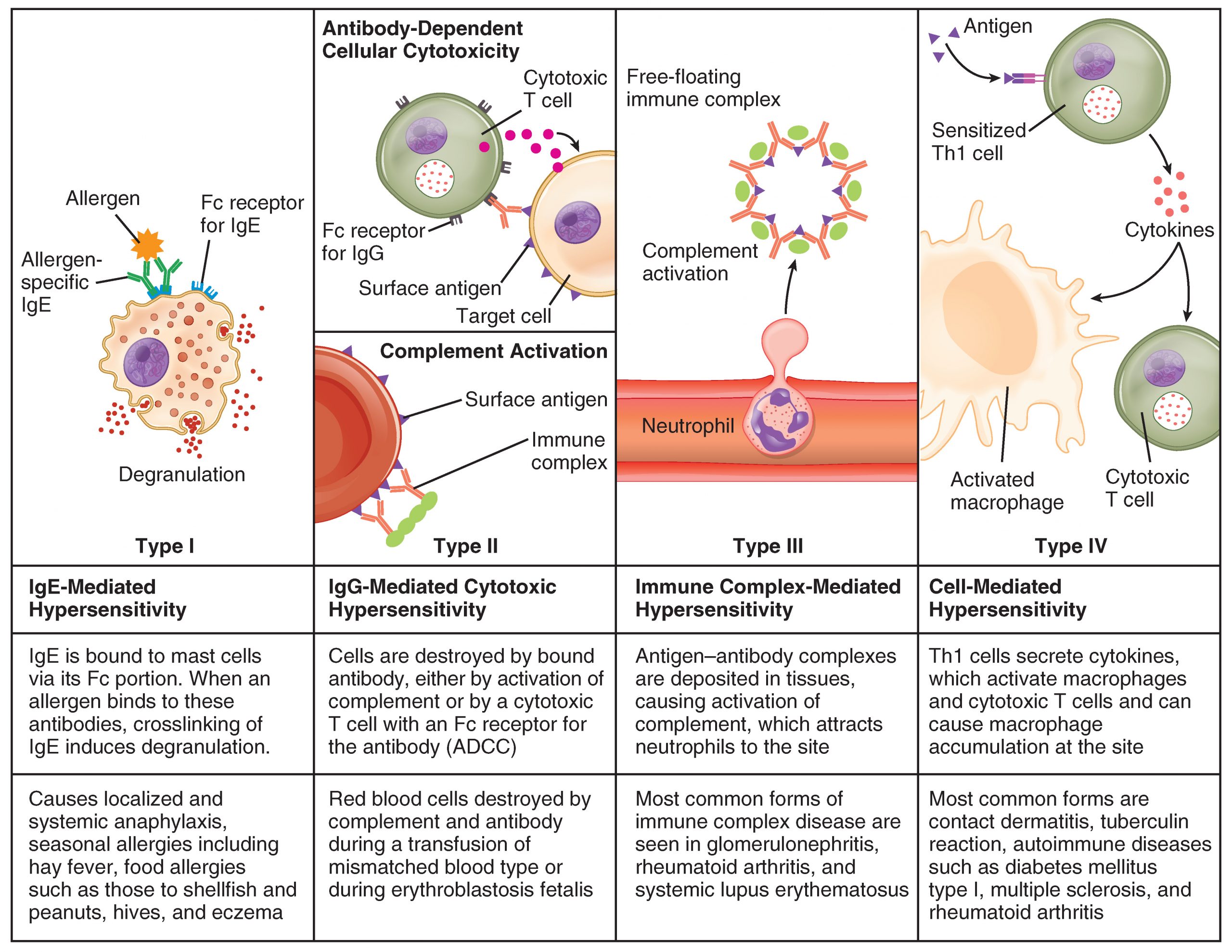
Immediate (Type I) Hypersensitivity
Antigens that cause allergic responses are often referred to as allergens. The specificity of the immediate hypersensitivity response is predicated on the binding of allergen-specific IgE to the mast cell surface. The process of producing allergen-specific IgE is called sensitization, and is a necessary prerequisite for the symptoms of immediate hypersensitivity to occur. Allergies and allergic asthma are mediated by mast cell degranulation that is caused by the crosslinking of the antigen-specific IgE molecules on the mast cell surface. The mediators released have various vasoactive effects already discussed, but the major symptoms of inhaled allergens are the nasal edema and runny nose caused by the increased vascular permeability and increased blood flow of nasal blood vessels. As these mediators are released with mast cell degranulation, type I hypersensitivity reactions are usually rapid and occur within just a few minutes, hence the term immediate hypersensitivity.
Most allergens are in themselves nonpathogenic and therefore innocuous. Some individuals develop mild allergies, which are usually treated with antihistamines. Others develop severe allergies that may cause anaphylactic shock, which can potentially be fatal within 20 to 30 minutes if untreated. This drop in blood pressure (shock) with accompanying contractions of bronchial smooth muscle is caused by systemic mast cell degranulation when an allergen is eaten (for example, shellfish and peanuts), injected (by a bee sting or being administered penicillin), or inhaled (asthma). Because epinephrine raises blood pressure and relaxes bronchial smooth muscle, it is routinely used to counteract the effects of anaphylaxis and can be lifesaving. Patients with known severe allergies are encouraged to keep automatic epinephrine injectors with them at all times, especially when away from easy access to hospitals.
Allergists use skin testing to identify allergens in type I hypersensitivity. In skin testing, allergen extracts are injected into the epidermis, and a positive result of a soft, pale swelling at the site surrounded by a red zone (called the wheal and flare response), caused by the release of histamine and the granule mediators, usually occurs within 30 minutes. The soft center is due to fluid leaking from the blood vessels and the redness is caused by the increased blood flow to the area that results from the dilation of local blood vessels at the site.
Type II and Type III Hypersensitivities
Type II hypersensitivity, which involves IgG-mediated lysis of cells by complement proteins, occurs during mismatched blood transfusions and blood compatibility diseases such as erythroblastosis fetalis (see section on transplantation). Type III hypersensitivity occurs with diseases such as systemic lupus erythematosus, where soluble antigens, mostly DNA and other material from the nucleus, and antibodies accumulate in the blood to the point that the antigen and antibody precipitate along blood vessel linings. These immune complexes often lodge in the kidneys, joints, and other organs where they can activate complement proteins and cause inflammation.
Delayed (Type IV) Hypersensitivity
Delayed hypersensitivity, or type IV hypersensitivity, is basically a standard cellular immune response. In delayed hypersensitivity, the first exposure to an antigen is called sensitization, such that on re-exposure, a secondary cellular response results, secreting cytokines that recruit macrophages and other phagocytes to the site. These sensitized T cells, of the Th1 class, will also activate cytotoxic T cells. The time it takes for this reaction to occur accounts for the 24- to 72-hour delay in development.
The classical test for delayed hypersensitivity is the tuberculin test for tuberculosis, where bacterial proteins from M. tuberculosis are injected into the skin. A couple of days later, a positive test is indicated by a raised red area that is hard to the touch, called an induration, which is a consequence of the cellular infiltrate, an accumulation of activated macrophages. A positive tuberculin test means that the patient has been exposed to the bacteria and exhibits a cellular immune response to it.
Another type of delayed hypersensitivity is contact sensitivity, where substances such as the metal nickel cause a red and swollen area upon contact with the skin. The individual must have been previously sensitized to the metal. A much more severe case of contact sensitivity is poison ivy, but many of the harshest symptoms of the reaction are associated with the toxicity of its oils and are not T cell mediated.
Autoimmune Responses
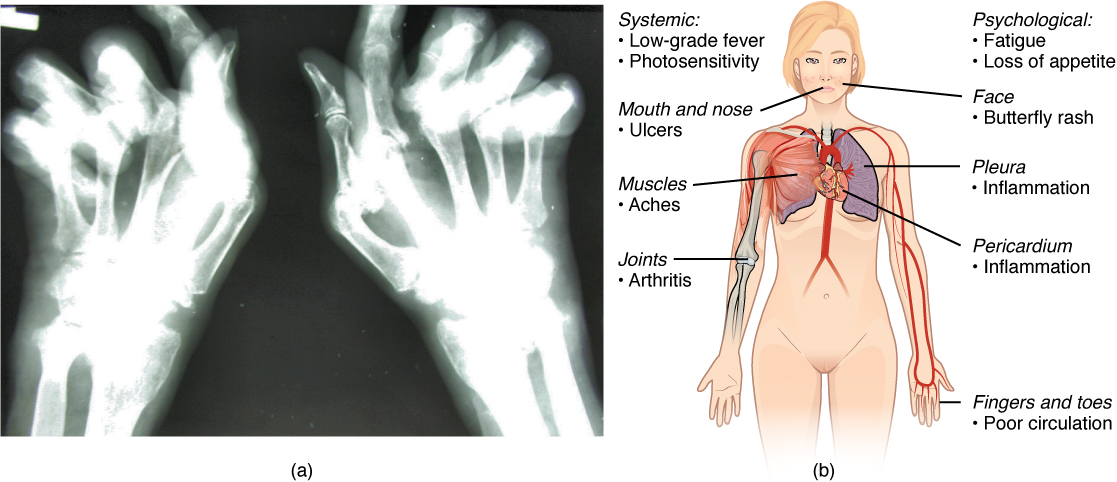
The worst cases of the immune system over-reacting are autoimmune diseases. Somehow, tolerance breaks down and the immune systems in individuals with these diseases begin to attack their own bodies, causing significant damage. The trigger for these diseases is, more often than not, unknown, and the treatments are usually based on resolving the symptoms using immunosuppressive and anti-inflammatory drugs such as steroids. These diseases can be localized and crippling, as in rheumatoid arthritis, or diffuse in the body with multiple symptoms that differ in different individuals, as is the case with systemic lupus erythematosus (Figure 21.6.2).
Environmental triggers seem to play large roles in autoimmune responses. One explanation for the breakdown of tolerance is that, after certain bacterial infections, an immune response to a component of the bacterium cross-reacts with a self-antigen. This mechanism is seen in rheumatic fever, a result of infection with Streptococcus bacteria, which causes strep throat. The antibodies to this pathogen’s M protein cross-react with an antigenic component of heart myosin, a major contractile protein of the heart that is critical to its normal function. The antibody binds to these molecules and activates complement proteins, causing damage to the heart, especially to the heart valves. On the other hand, some theories propose that having multiple common infectious diseases actually prevents autoimmune responses. The fact that autoimmune diseases are rare in countries that have a high incidence of infectious diseases supports this idea, another example of the hygiene hypothesis discussed earlier in this chapter.
There are genetic factors in autoimmune diseases as well. Some diseases are associated with the MHC genes that an individual expresses. The reason for this association is likely because if one’s MHC molecules are not able to present a certain self-antigen, then that particular autoimmune disease cannot occur. Overall, there are more than 80 different autoimmune diseases, which are a significant health problem in the elderly. Table 21.7 lists several of the most common autoimmune diseases, the antigens that are targeted, and the segment of the adaptive immune response that causes the damage.
| Autoimmune Diseases (Table 21.7) | ||
|---|---|---|
| Disease | Autoantigen | Symptoms |
| Celiac disease | Tissue transglutaminase | Damage to small intestine |
| Diabetes mellitus type I | Beta cells of pancreas | Low insulin production; inability to regulate serum glucose |
| Graves’ disease | Thyroid-stimulating hormone receptor (antibody blocks receptor) | Hyperthyroidism |
| Hashimoto’s thyroiditis | Thyroid-stimulating hormone receptor (antibody mimics hormone and stimulates receptor) | Hypothyroidism |
| Lupus erythematosus | Nuclear DNA and proteins | Damage of many body systems |
| Myasthenia gravis | Acetylcholine receptor in neuromuscular junctions | Debilitating muscle weakness |
| Rheumatoid arthritis | Joint capsule antigens | Chronic inflammation of joints |
Chapter Review
The immune response can be under-reactive or over-reactive. Suppressed immunity can result from inherited genetic defects or by acquiring viruses. Over-reactive immune responses include the hypersensitivities: B cell- and T cell-mediated immune responses designed to control pathogens, but that lead to symptoms or medical complications. The worst cases of over-reactive immune responses are autoimmune diseases, where an individual’s immune system attacks his or her own body because of the breakdown of immunological tolerance. These diseases are more common in the aged, so treating them will be a challenge in the future as the aged population in the world increases.
Review Questions
Critical Thinking Questions
1. Describe anaphylactic shock in someone sensitive to peanuts?
2. Describe rheumatic fever and how tolerance is broken.
Glossary
- delayed hypersensitivity
- (type IV) T cell-mediated immune response against pathogens infiltrating interstitial tissues, causing cellular infiltrate
- immediate hypersensitivity
- (type I) IgE-mediated mast cell degranulation caused by crosslinking of surface IgE by antigen
- sensitization
- first exposure to an antigen
- severe combined immunodeficiency disease (SCID)
- genetic mutation that affects both T cell and B cell arms of the immune response
- type I hypersensitivity
- immediate response mediated by mast cell degranulation caused by the crosslinking of the antigen-specific IgE molecules on the mast cell surface
- type II hypersensitivity
- cell damage caused by the binding of antibody and the activation of complement, usually against red blood cells
- type III hypersensitivity
- damage to tissues caused by the deposition of antibody-antigen (immune) complexes followed by the activation of complement
Solutions
Answers for Critical Thinking Questions
- The peanuts cause high levels of mast cell degranulation in the throats of these individuals. The histamine released increases vascular permeability, causing edema and (swelling), making breathing difficult. This must be treated with epinephrine as soon as possible.
- Antibody response to the cell walls of β-Streptococcus cross-reacts with the heart muscle. Complement is then activated and the heart is damaged, leading to abnormal function. Tolerance is broken because heart myosin antigens are similar to antigens on the β- Streptococcus bacteria.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.

