27.1 Anatomy of Sexual Systems
Learning Objectives
By the end of this section, you will be able to:
- Describe the structure and general functions of the organs of sexual systems
Introduction
In this section we describe the anatomy at either extreme of the spectrum of sexual anatomical variation. In section 27.2, we will describe the variations of sexual anatomy that occur which are not easily characterized by this binary system of male or female.
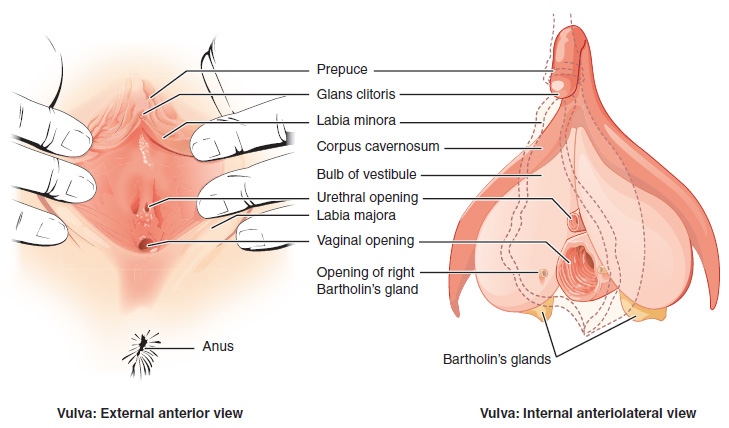
Vulva
The mons pubis is a pad of fat that is located over the pubic bone. After puberty, it becomes covered in pubic hair. The labia majora (labia = “lips”; majora = “larger”) are folds of pubic hair-covered skin that extend from the mons pubis to the perineal raphe – the region of skin between the vaginal opening and the anus. The thinner and more pigmented labia minora (labia = “lips”; minora = “smaller”) are medial to the labia majora. The labia majora and minora naturally vary in shape and size from person to person, and left-right asymmetries are normal and expected. The vestibule is the region between the two labia minora. Therefore, the labia minora protect the mucous membranes and orifices of the urethra and vagina, found in the vestibule. The mons pubis, labia majora, labia minora and vestibule are collectively referred to as the vulva (Figure 27.1.1).
Clitoris
The superior, anterior portions of the labia minora come together to meet the glans of the clitoris which has an extremely dense network of nerve endings. This is the portion of the clitoris that is partially covered by the prepuce (foreskin) of the clitoris. The clitoris also includes crura or legs (sing.: crus or leg) which are subcutaneous and extend inferiorly, following the contours of the pubic rami. The glans and crura are connected by the body of the clitoris. The glans, crura and body of the clirtoris are made up of corpus cavernosum erectile tissue. In contrast, the bulbs of the vestibule are corpus spongiosum erectile tissue. It is found medial to the crura of the clitoris and surrounds the vaginal and urethral orifices. The non-erect clitoris (including the superficial glans through to the end of the subcutaneous crura) has been recorded to be as long as 9 cm.
The Female Prostate
Surrounding the urethra is glandular tissue that has been called the periurethral gland, the paraurethral gland, the lesser vestibular gland and the female prostate. These glands were first identified in the 1600’s, then appear again in the anatomical literature of the 1800’s, and in 2002 the Federative International Programme for Anatomical Terminology committee officially voted to use the term “female prostate” to describe these glands that surround the urethra, which release the fluids of female ejaculation. As with all anatomy, there is a degree of variation in regard to the size, number and location of the ducts leading from the female prostate, but the ducts typically lead to the distal portion of the urethra.
Greater Vestibular Glands
The paired greater vestibular glands (Bartholin’s glands) are located inferior and posterior to the bulbs of the vestibule. The glands secrete mucous into the vestibular area through ducts which open on either side of the vaginal orifice.
Vagina
The vagina (Figure 27.1.3) is a muscular canal (approximately 10 cm long) typically leading to the uterus. The superior portion of the vagina—called the fornix—meets the protruding uterine cervix. The walls of the vagina are lined with an outer fibrous adventitia; a middle layer of smooth muscle; and an inner mucous membrane with transverse folds called rugae. Together, the middle and inner layers allow the expansion of the vagina. The vaginal opening is located between the opening of the urethra and the anus. The hymen is a thin membrane that sometimes partially covers the entrance to the vagina. An intact hymen cannot be used as an indication of “virginity”; even at birth, this is only a partial membrane, as menstrual fluid and other secretions must be able to exit the body. The opening between the hymen and the vaginal wall can change in size based on the degree in which the hymen is stretched. The membrane will decrease in size due to increased pressure.
The vagina is home to a normal population of microorganisms that help to protect against infection by pathogenic bacteria, yeast, or other organisms that can enter the vagina. In a healthy vagina, the most predominant type of bacteria is from the genus Lactobacillus. This family of beneficial bacterial flora secretes lactic acid, and thus protects the vagina by maintaining an acidic pH (below 4.5). Potential pathogens are less likely to survive in these acidic conditions. Lactic acid, in combination with other vaginal secretions, makes the vagina a self-cleansing organ. Douching (washing out the vagina with fluid) disrupts the normal balance of healthy microorganisms, and increases the risk for infections and irritation. Indeed, the American College of Obstetricians and Gynecologists recommends against douching, and instead recommends allowing the vagina to maintain its normal healthy population of protective microbial flora.
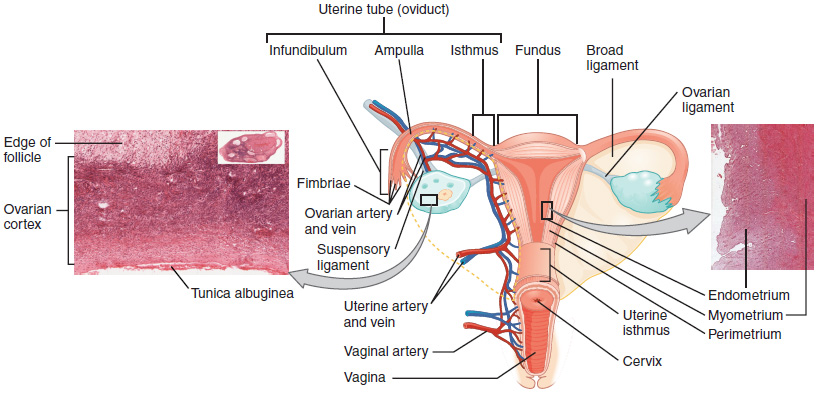
Uterus
The uterus is a muscular organ with an average size 5 cm wide by 7 cm long. It has three regions. The portion of the uterus superior to the opening of the uterine tubes is called the fundus. The middle section of the uterus is called the body. The cervix is the narrow inferior portion of the uterus that projects into the vagina. The cervix produces mucus secretions that vary in consistency and volume across the ovarian cycle. The cervix opens into the vaginal cavity via the os, which allows cervical fluid to move through the vagina and exit the body through the vaginal opening.
Several ligaments maintain the position of the uterus within the abdominopelvic cavity. The broad ligament is a fold of peritoneum extending laterally from both sides of the uterus and attaching it to the pelvic wall. The round ligament attaches to the uterus near the uterine tubes, and extends to the labia majora. Finally, the uterosacral ligament stabilizes the uterus posteriorly by its connection from the cervix to the pelvic wall.
The wall of the uterus is made up of three layers. The most superficial layer is the serous membrane, or perimetrium, which consists of epithelial tissue that covers the exterior portion of the uterus. The middle layer, or myometrium, is a thick layer of smooth muscle responsible for uterine contractions. Most of the uterus is myometrial tissue, and the muscle fibers run horizontally, vertically, and diagonally, allowing the contractions that occur during orgasm labor or menstruation.
The innermost layer of the uterus is called the endometrium. The endometrium consists of two layers: the stratum basalis and the stratum functionalis (the basal and functional layers).
The uterine tubes (also called Fallopian tubes) serve as the conduit of the oocyte from the ovary to the uterus. The uterine tubes are divided into multiple regions. The isthmus is the narrow medial end of each uterine tube that is connected to the uterus. The middle region of the tube is called the ampulla. The wide distal infundibulum flares out with slender, finger-like projections called fimbriae. The uterine tubes also have three layers: an outer serosa, a middle smooth muscle layer, and an inner mucosal layer. In addition to its mucus-secreting cells, the inner mucosa contains ciliated cells that beat in the direction of the uterus, producing a current that will be critical to move the oocyte.
The open-ended structure of the uterine tubes can have significant health consequences if bacteria or other contagions enter through the vagina and move through the uterus, into the tubes, and then into the pelvic cavity. If this is left unchecked, a bacterial infection (sepsis) could quickly become life-threatening. The spread of an infection in this manner is of special concern when unskilled practitioners perform abortions in non-sterile conditions. Sepsis is also associated with sexually transmitted bacterial infections, especially gonorrhea and chlamydia. These increase the risk for pelvic inflammatory disease (PID), infection of the uterine tubes or other reproductive organs. Even when resolved, PID can leave scar tissue in the tubes, leading to infertility.
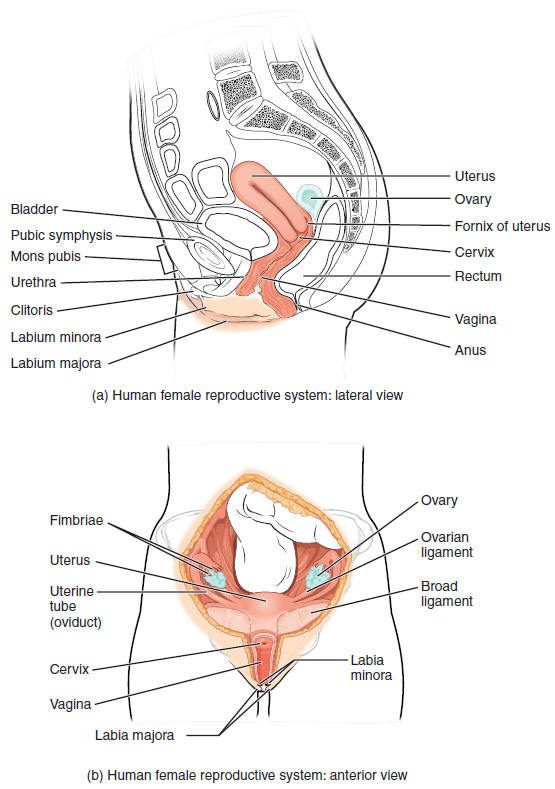
Ovaries
The ovaries are the gonads (see Figure 27.1.3) located at the distal end of the uterine tubes, close to the fimbriae. They are each about 2 to 3 cm in length, about the size of an almond. The ovaries are supported by the mesovarium, a double fold of peritoneum that is part of the broad ligament. The suspensory ligament is the peritoneum that contains the ovarian blood and lymph vessels. The ovary itself is attached to the uterus via the ovarian ligament.
The ovary comprises an outer covering of cuboidal epithelium that is superficial to a dense connective tissue covering called the tunica albuginea. Beneath the tunica albuginea is the cortex, or outer portion, of the organ. The cortex is composed of a tissue framework called the ovarian stroma that forms the bulk of the adult ovary.
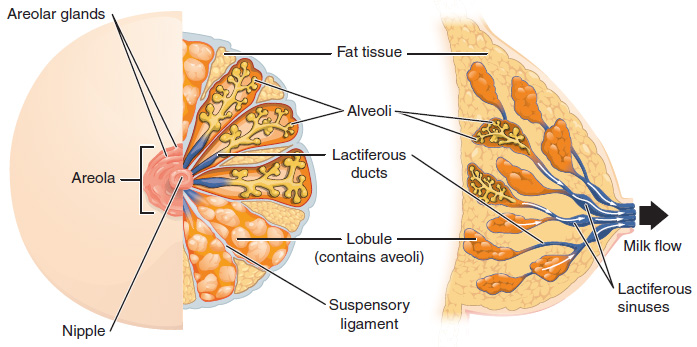
Breasts
The external features of the breast include a nipple surrounded by a pigmented areola (Figure 27.1.4), whose coloration may deepen due to changes in hormone levels. The areola is typically circular and can vary in size from 25 to 100 mm in diameter. The areolar region is characterized by small, raised areolar glands that secrete lubricating fluid under certain hormonal conditions.
Breast milk is produced by the mammary glands, which are modified sweat glands. The milk itself exits the breast through the nipple via 15 to 20 lactiferous ducts that open on the surface of the nipple. These lactiferous ducts each extend to a lactiferous sinus that connects to a glandular lobe within the breast itself that contains groups of milk-secreting cells in clusters called alveoli (see Figure 27.1.4). The clusters can change in size depending on the amount of milk in the alveolar lumen. Once milk is made in the alveoli, stimulated myoepithelial cells that surround the alveoli contract to push the milk to the lactiferous sinuses. From here, milk can be drawn through the lactiferous ducts by suckling. The lobes themselves are surrounded by fat tissue, which determines the size of the breast; breast size differs between individuals and does not affect the amount of milk produced. Asymmetry in breast size within an individual is expected and normal. Increased levels of hormones can lead to further development of the mammary tissue and enlargement of the breasts. Supporting the breasts are multiple bands of connective tissue called suspensory ligaments that connect the breast tissue to the dermis of the overlying skin.
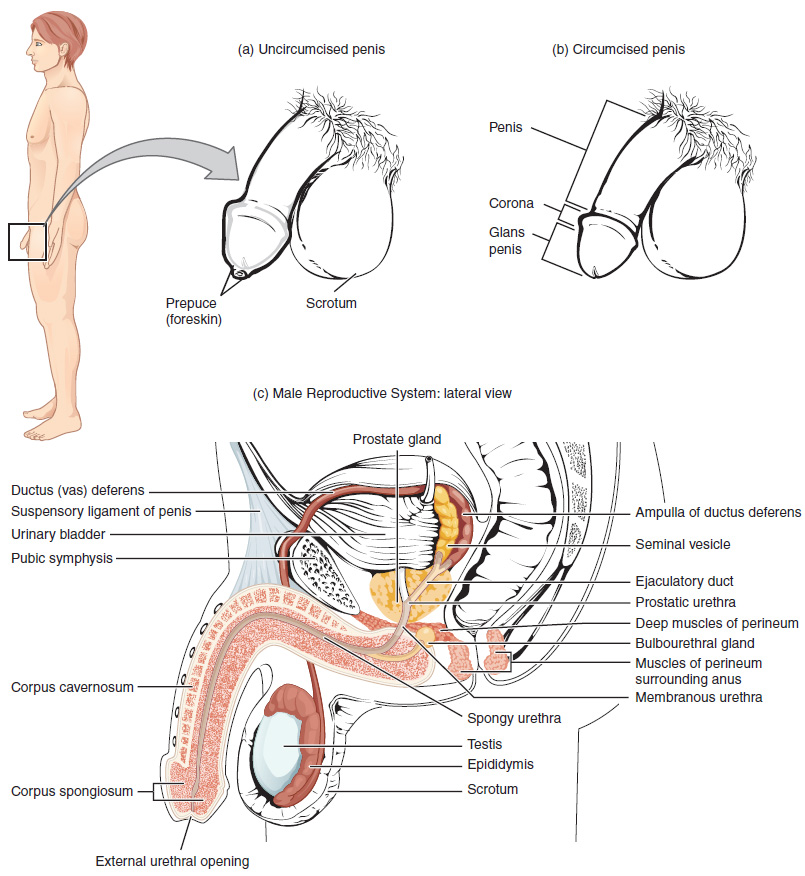
The Penis
The penis is flaccid for non-sexual actions, such as urination, and turgid and erect during sexual arousal. The shaft of the penis surrounds the urethra (Figure 27.1.5). The shaft is composed of three column-like chambers of erectile tissue that span the length of the shaft. Each of the two larger lateral chambers is called a corpus cavernosum (plural = corpora cavernosa). Together, these make up the bulk of the penis. The corpus spongiosum, a raised ridge on the erect penis, is a smaller chamber that surrounds the spongy, or penile, urethra. The end of the penis, called the glans penis, has a high concentration of nerve endings, however not as dense and therefore not as sensitive as the glans clitoris (see Figure 27.1.5). The skin from the shaft extends down over the glans and forms a collar called the prepuce (or foreskin). The foreskin also contains a dense concentration of nerve endings, and both lubricates and protects the sensitive skin of the glans penis. A surgical procedure called circumcision, often performed for religious or social reasons, removes the prepuce, typically within days of birth. The skin of the glans of a circumcised penis converts from a mucous membrane to a cutaneous membrane, and the friction reducing function of the foreskin is lost.
Testes
The testes (singular = testis) are the gonads which produce both sperm and androgens, such as testosterone, and are active throughout the sexual lifespan. The testes are spherical in shape, each approximately 4 to 5 cm in length and are housed within the scrotum (see Figure 27.1.7). They are surrounded by two distinct layers of protective connective tissue (Figure 27.1.6). The outer tunica vaginalis is a serous membrane that has both a parietal and a thin visceral layer (similar to the visceral and parietal serous membranes of the pericardium, peritoneum, and pleura). Beneath the tunica vaginalis is the tunica albuginea, a tough, white, dense connective tissue layer covering the testis itself. Not only does the tunica albuginea cover the outside of the testis, it also invaginates to form septa that divide the testis into 300 to 400 structures called lobules. Within the lobules, sperm develop in structures called seminiferous tubules. During the seventh month of the developmental period of a fetus secreting testosterone, each testis moves through the abdominal musculature to descend into the scrotal cavity. This is called the “descent of the testis.” Cryptorchidism is the clinical term used when one or both of the testes fail to descend into the scrotum prior to birth.
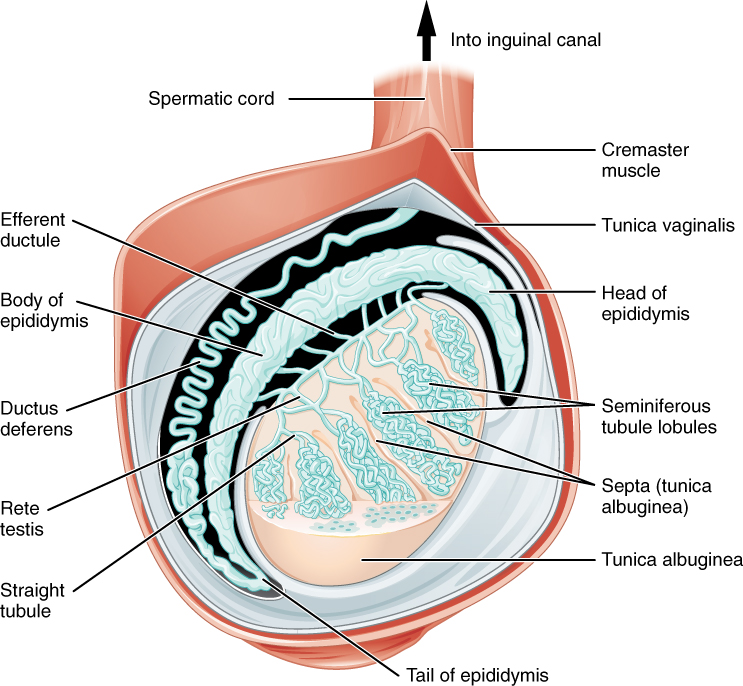
The tightly coiled seminiferous tubules form the bulk of each testis. Within the tubules are developing sperm cells. From the lumens of the seminiferous tubules, sperm move into the straight tubules (or tubuli recti), and from there into a fine meshwork of tubules called the rete testes. Sperm leave the rete testes, and the testis itself, through the 15 to 20 efferent ductules that cross the tunica albuginea.
Inside the seminiferous tubules are six different cell types. These include supporting cells called sustentacular cells, as well as five types of developing sperm cells called germ cells. Germ cell development progresses from the basement membrane—at the perimeter of the tubule—toward the lumen.
Epididymis
From the lumen of the seminiferous tubules, the immotile sperm are surrounded by testicular fluid and moved to the epididymis (plural = epididymides), a coiled tube attached to the testis where newly formed sperm continue to mature (see Figure 27.1.6) Though the epididymis does not take up much room in its tightly coiled state, it would be approximately 6 m (20 feet) long if straightened. It takes an average of 12 days for sperm to move through the coils of the epididymis, with the shortest recorded transit time in humans being one day. Sperm enter the head of the epididymis and are moved along predominantly by the contraction of smooth muscles lining the epididymal tubes. As they are moved along the length of the epididymis, the sperm further mature and acquire the ability to move on their own. The more mature sperm are then stored in the tail of the epididymis (the final section) until ejaculation occurs.
Scrotum
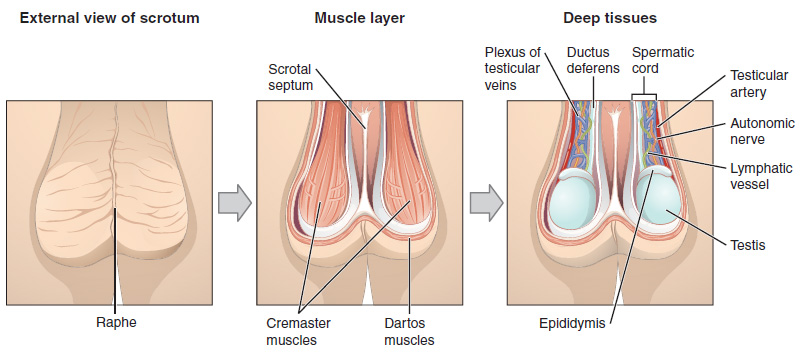
The testes are located in a skin-covered, highly pigmented, muscular sack called the scrotum that extends from the body behind the penis (see Figure 27.1.5). This location is important in sperm production, which occurs within the testes, and proceeds more efficiently when the testes are kept 2 to 4°C below core body temperature.
The dartos muscle makes up the subcutaneous muscle layer of the scrotum (Figure 27.1.7). It continues internally to make up the scrotal septum, a wall that divides the scrotum into two compartments, each housing one testis. Descending from the internal oblique muscle of the abdominal wall are the two cremaster muscles, which cover each testis like a muscular net. By contracting simultaneously, the dartos and cremaster muscles can elevate the testes in cold weather (or water), moving the testes closer to the body and decreasing the surface area of the scrotum to retain heat. Alternatively, as the environmental temperature increases, the scrotum relaxes, moving the testes farther from the body core and increasing scrotal surface area, which promotes heat loss. Externally, the scrotum has a raised medial thickening on the surface called the raphae.
Duct System
During ejaculation, sperm exit the tail of the epididymis and are pushed by smooth muscle contraction to the ductus deferens (also called the vas deferens). The ductus deferens is a thick, muscular tube that is bundled together inside the scrotum with connective tissue, blood vessels, and nerves into a structure called the spermatic cord (see Figure 27.1.5 and Figure 27.1.7). Because the ductus deferens is physically accessible within the scrotum, surgical sterilization to interrupt ejaculation of sperm can be performed by cutting and sealing a small section of the ductus (vas) deferens. This procedure is called a vasectomy, and it is an effective form of birth control. Although it may be possible to reverse a vasectomy, clinicians consider the procedure permanent.
External Website

Watch this video to learn about a vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This interrupts the path taken by sperm through the ductus deferens. If sperm do not exit through the vas, either because the person has had a vasectomy or has not ejaculated, in what region of the testis do they remain?
Each ductus deferens extends superiorly into the abdominal cavity through the inguinal canal in the abdominal wall. From here, the ductus deferens continues to the pelvic cavity, ending posterior to the bladder where it dilates in a region called the ampulla (meaning “flask”).
Sperm make up only 5 percent of the final volume of semen, the thick, milky fluid that is ejaculated. The bulk of semen is produced by three critical accessory glands of the sexual system: the seminal vesicles, the prostate, and the bulbourethral glands.
Seminal Vesicles
As sperm pass through the ampulla of the ductus deferens at ejaculation, they mix with fluid from the associated seminal vesicle (see Figure 27.1.5). The paired seminal vesicles are glands that contribute approximately 60 percent of the semen volume. Seminal vesicle fluid contains large amounts of fructose, which is used by the sperm mitochondria to generate ATP to allow movement.
The fluid, now containing both sperm and seminal vesicle secretions, next moves into the associated ejaculatory duct, a short structure formed from the ampulla of the ductus deferens and the duct of the seminal vesicle. The paired ejaculatory ducts transport the seminal fluid into the next structure, the prostate gland.
Prostate Gland
As shown in Figure 27.1.5, the centrally located prostate gland sits anterior to the rectum at the base of the bladder surrounding the prostatic urethra (the portion of the urethra that runs within the prostate). About the size of a walnut, the prostate is formed of both muscular and glandular tissues. It excretes an alkaline, milky fluid to the passing seminal fluid, now called semen.
Bulbourethral Glands
The final addition to semen is made by two bulbourethral glands (or Cowper’s glands) that release a thick fluid that lubricates the urethra, and helps to neutralize urine residues from the penile urethra. The fluid from these glands is released after the male becomes sexually aroused, and shortly before the release of the semen. It is referred to as pre-ejaculate.
Disorders of the Prostate gland
At approximately age 25, the prostate gradually begins to enlarge. This enlargement does not usually cause problems; however, abnormal growth of the prostate, or benign prostatic hyperplasia (BPH), can cause constriction of the urethra as it passes through the middle of the prostate gland, leading to a number of lower urinary tract symptoms, such as a frequent and intense urge to urinate, a weak stream, and a sensation that the bladder has not emptied completely. The number of individuals with BPH increases dramatically with age. Treatments for BPH attempt to relieve the pressure on the urethra so that urine can flow more normally. Mild to moderate symptoms are treated with medication, whereas severe enlargement of the prostate is treated by surgery in which a portion of the prostate tissue is removed.
Another common disorder involving the prostate is prostate cancer. According to the Centers for Disease Control and Prevention (CDC), prostate cancer is one of the most common cancers. However, some forms of prostate cancer grow very slowly and thus may not ever require treatment. Aggressive forms of prostate cancer, in contrast, involve metastasis to vulnerable organs like the lungs and brain. There is no link between BPH and prostate cancer, but the symptoms are similar. Prostate cancer is detected by a medical history, a blood test, and a rectal exam that allows physicians to palpate the prostate and check for unusual masses. If a mass is detected, the cancer diagnosis is confirmed by biopsy of the cells.
Chapter Review
This chapter outlined the anatomical features of the extremes of the spectrum of sexual anatomy, the binary male or female. There are numerous reasons why someone may not experience their sexual anatomy in one or the other of these binary frameworks – including, but not limited to, unique anatomical development, or surgical changes. The following chapter will address development of sexual anatomy.
Interactive Link Questions
Watch this video to learn about vasectomy. As described in this video, a vasectomy is a procedure in which a small section of the ductus (vas) deferens is removed from the scrotum. This interrupts the path taken by sperm through the ductus deferens. If sperm do not exit through the vas, either because the man has had a vasectomy or has not ejaculated, in what region of the testis do they remain?
Sperm remain in the epididymis until they degenerate.
Watch this video to explore the structures of the male reproductive system and the path of sperm that starts in the testes and ends as the sperm leave the penis through the urethra. Where are sperm deposited after they leave the ejaculatory duct?
Sperm enter the prostate.
Review Questions
Critical Thinking Questions
1. Briefly explain why mature gametes carry only one set of chromosomes.
2. What special features are evident in sperm cells but not in somatic cells, and how do these specializations function?
3. What do each of the three male accessory glands contribute to the semen?
4. Describe how penile erection occurs.
5. While anabolic steroids (synthetic testosterone) bulk up muscles, they can also affect testosterone production in the testis. Using what you know about negative feedback, describe what would happen to testosterone production in the testis if a male takes large amounts of synthetic testosterone.
Glossary
- blood–testis barrier
- tight junctions between Sertoli cells that prevent bloodborne pathogens from gaining access to later stages of spermatogenesis and prevent the potential for an autoimmune reaction to haploid sperm
- bulbourethral glands
- (also, Cowper’s glands) glands that secrete a lubricating mucus that cleans and lubricates the urethra prior to and during ejaculation
- corpus cavernosum
- either of two columns of erectile tissue in the penis that fill with blood during an erection
- corpus spongiosum
- (plural = corpora cavernosa) column of erectile tissue in the penis that fills with blood during an erection and surrounds the penile urethra on the ventral portion of the penis
- ductus deferens
- (also, vas deferens) duct that transports sperm from the epididymis through the spermatic cord and into the ejaculatory duct; also referred as the vas deferens
- ejaculatory duct
- duct that connects the ampulla of the ductus deferens with the duct of the seminal vesicle at the prostatic urethra
- epididymis
- (plural = epididymides) coiled tubular structure in which sperm start to mature and are stored until ejaculation
- gamete
- haploid reproductive cell that contributes genetic material to form an offspring
- glans penis
- bulbous end of the penis that contains a large number of nerve endings
- gonadotropin-releasing hormone (GnRH)
- hormone released by the hypothalamus that regulates the production of follicle-stimulating hormone and luteinizing hormone from the pituitary gland
- gonads
- reproductive organs (testes in men and ovaries in women) that produce gametes and reproductive hormones
- inguinal canal
- opening in abdominal wall that connects the testes to the abdominal cavity
- Leydig cells
- cells between the seminiferous tubules of the testes that produce testosterone; a type of interstitial cell
- penis
- male organ of copulation
- prepuce
- (also, foreskin) flap of skin that forms a collar around, and thus protects and lubricates, the glans penis; also referred as the foreskin
- prostate gland
- doughnut-shaped gland at the base of the bladder surrounding the urethra and contributing fluid to semen during ejaculation
- scrotum
- external pouch of skin and muscle that houses the testes
- semen
- ejaculatory fluid composed of sperm and secretions from the seminal vesicles, prostate, and bulbourethral glands
- seminal vesicle
- gland that produces seminal fluid, which contributes to semen
- seminiferous tubules
- tube structures within the testes where spermatogenesis occurs
- Sertoli cells
- cells that support germ cells through the process of spermatogenesis; a type of sustentacular cell
- sperm
- (also, spermatozoon) male gamete
- spermatic cord
- bundle of nerves and blood vessels that supplies the testes; contains ductus deferens
- spermatid
- immature sperm cells produced by meiosis II of secondary spermatocytes
- spermatocyte
- cell that results from the division of spermatogonium and undergoes meiosis I and meiosis II to form spermatids
- spermatogenesis
- formation of new sperm, occurs in the seminiferous tubules of the testes
- spermatogonia
- (singular = spermatogonium) diploid precursor cells that become sperm
- spermiogenesis
- transformation of spermatids to spermatozoa during spermatogenesis
- testes
- (singular = testis) male gonads
Solutions
Answers for Critical Thinking Questions
- A single gamete must combine with a gamete from an individual of the opposite sex to produce a fertilized egg, which has a complete set of chromosomes and is the first cell of a new individual.
- Unlike somatic cells, sperm are haploid. They also have very little cytoplasm. They have a head with a compact nucleus covered by an acrosome filled with enzymes, and a mid-piece filled with mitochondria that power their movement. They are motile because of their tail, a structure containing a flagellum, which is specialized for movement.
- The three accessory glands make the following contributions to semen: the seminal vesicle contributes about 60 percent of the semen volume, with fluid that contains large amounts of fructose to power the movement of sperm; the prostate gland contributes substances critical to sperm maturation; and the bulbourethral glands contribute a thick fluid that lubricates the ends of the urethra and the vagina and helps to clean urine residues from the urethra.
- During sexual arousal, nitric oxide (NO) is released from nerve endings near blood vessels within the corpora cavernosa and corpus spongiosum. The release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the penile arteries, causing them to dilate. This dilation increases the amount of blood that can enter the penis, and induces the endothelial cells in the penile arterial walls to secrete NO, perpetuating the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled penile venules, preventing venous drainage of the penis. An erection is the result of this increased blood flow to the penis and reduced blood return from the penis.
- Testosterone production by the body would be reduced if a male were taking anabolic steroids. This is because the hypothalamus responds to rising testosterone levels by reducing its secretion of GnRH, which would in turn reduce the anterior pituitary’s release of LH, finally reducing the manufacture of testosterone in the testes.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.

