27.5 Physiology of Arousal and Orgasm
Learning Objectives
By the end of this section, you will be able to:
- Explain how bipotential tissues are directed to develop into male or female sex organs
- Name the rudimentary duct systems in the embryo that are precursors to male or female internal sex organs
- Describe the hormonal changes that bring about puberty, and the secondary sex characteristics of men and women
Introduction:
The following chapter will discuss the physiology of arousal and orgasm. Arousal includes the physiology of erection and increased lubrication production due to a combination of mental and physical stimuli. Orgasm typically includes the release of ejaculate and involuntary muscle contractions accompanied by feelings of euphoria. Immediately following orgasm there is resolution of vasocongestion in erectile tissue followed by feelings of contentment and relaxation.
Arousal:
The physiological process of arousal can begin due to sexual thoughts or from physical stimulation. Mostly commonly, the combination of mental and physical input together – synapsing with the sacral nerves roots – leads to reflexive patterns of physiologic arousal. Due to the reflexive nature of the response, positive mental stimulation is it not a requirement for physical signs of arousal to occur. Also, in the case of spinal cord injury, the location of the injury relative to the sacral nerve roots will dictate whether input from the brain, or from physical stimulation, will lead to physical signs of arousal. Sexual sensations are typically most intense due to physical stimulation of the glans of the clitoris or penis, although arousal can also occur due to stimulation of the nipples, all portions of the clitoris and penis, the vulva and perineal region, prostate, urethra, bladder, anal epithelium, scrotum, testes and vas deferens. Efferent and afferent signals related to sexual arousal travel along many nerves including the pudendal, pelvic splanchnic, hypogastric, vagus, ilioinguinal, posterior femoral cutaneous and genital branch of the genitofemoral nerve.
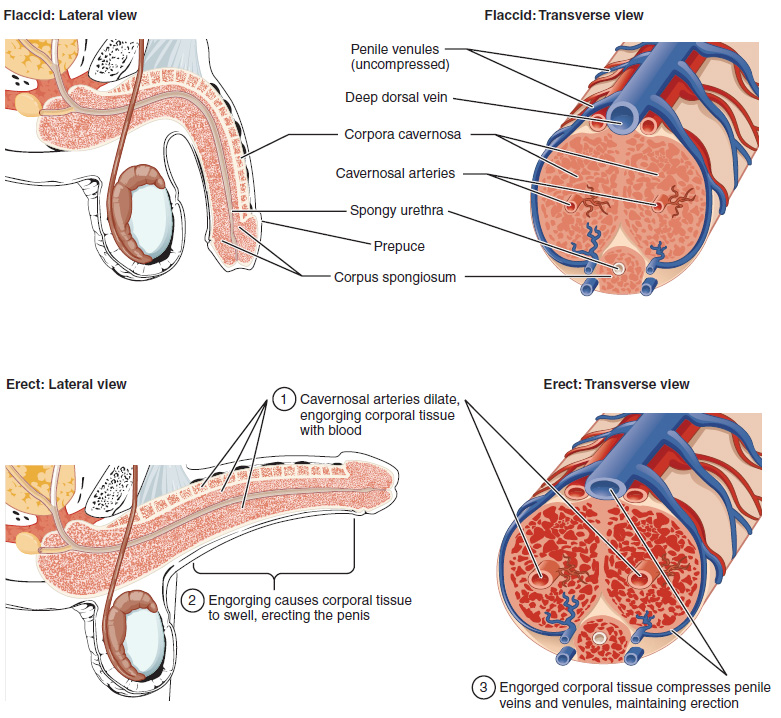
The clitoris, the bulbs of the vestibule and the penis are erectile tissues. Erections are the result of vasocongestion, or engorgement of the tissues because of more arterial blood flowing into the erectile structure than is leaving in the veins. During sexual arousal, nitric oxide (NO) is released from parasympathetic nerve endings near blood vessels within the corpora cavernosa and spongiosum. Release of NO activates a signaling pathway that results in relaxation of the smooth muscles that surround the arteries, causing them to dilate. This dilation increases the amount of blood that can enter the erectile structures and induces the endothelial cells in the arterial walls to also secrete NO and perpetuate the vasodilation. The rapid increase in blood volume fills the erectile chambers, and the increased pressure of the filled chambers compresses the thin-walled venules, preventing venous drainage. The result of this increased blood flow to the erectile structures, and reduced blood returning from the structure, is called erection.
Parasympathetic impulses during arousal cause the secretion of mucus from the greater vestibular glands into the vestibule of the vulva via a pair of ducts found lateral to the vaginal opening. Instead of mucus, the capillaries of the vaginal walls secrete serous fluid as vaginal lubrication. Arousal also causes the bulbourethral glands of the penis to release mucus into the urethra – which is referred to as pre-ejaculate or pre-cum. This release of mucus removes urine and old sperm from the urethra and provides lubrication for semen during ejaculation. If there has been a recent ejaculation, and the pre-ejaculate may have viable sperm in it.
Orgasm:
When the mental and/or physical stimuli have reached a necessary threshold, the spinal cord emits sympathetic impulses that lead to orgasm. Orgasm was defined by sex researcher Alfred Kinsey in 1953 as “The expulsive discharge of neuromuscular tensions at the peak of sexual response.” Others describe orgasm as climax or an altered state of consciousness. Neuroimaging studies have observed that during orgasm the prefrontal lobe and portions of the temporal lobe have decreased activity, while brain regions such as the nucleus accumbens (award center), amygdala (emotional center), hippocampus (memory), cerebellum (coordinated muscle tension) and hypothalamus (release of oxytocin) have an increased level of activity.
Overlaying the crus (legs) of the clitoris and penis are the ischiocavernosus muscles, while the bulbs of the vestibule and the bulb of the penis are covered by the bulbospongiosum. During orgasm, these involuntary muscles undergo rhythmic contraction, as do other perineal and pelvic and trunk muscles. There is evidence to suggest that the cervical canal dilates during orgasm, and that uterine motility is increased. Ejaculation through the urethra has the potential to occur in all individuals due to release of fluid from the prostate or female prostate. In some cases, ejaculation is retrograde, meaning that the fluid moves towards the bladder and may go undetected. The anatomical length of the urethra can influence the likelihood of retrograde ejaculation, and is more common in individuals with a short, rather than long, urethra. Contraction of the vas deferens and ampulla causes expulsion of sperm into the urethra, and contraction of the seminal vesicle and prostate add fluids to fill the urethral and produce reflective ejaculation of semen. The refractory period necessary between one orgasm and the next is highly variable and explains why some individuals can experience multiple orgasms, while others cannot.
The health benefits of orgasm have been investigated by some, and the results suggest that regular orgasm can improve sleep, decrease stress, decrease chronic pain, and decrease risk of incontinence and even mortality during aging. If sex will involve vaginal penetration, orgasms prior to penetration may be especially important to ensure that vaginal lubrication levels are sufficient to decrease the chance of laceration of the vaginal walls (vaginal laceration increases transmission of disease). There is also evidence to suggest that orgasms help decrease the chance of urinary tract infection following sexual activity due to the flushing of the urethra during ejaculation.
Resolution:
Within 1-2 minutes following orgasm, the resolution of the vasocongestion in the erectile tissues occurs (assuming cessation of the physical and/or mental stimuli, or inability for multiple orgasm due to the absolute refractory period). The smooth muscle of the artery walls is no longer relaxed due to NO release, and returns to its baseline vasomotor tone. This decreases the blood flow to the erectile tissues, equalizing the volume of blood entering and leaving the erectile chambers, and returning the structures to their non-erect size and shape. The hormones released upon orgasm, such as oxytocin, lead to the feelings of contentment and well being.
Erectile Dysfunction:
Erectile dysfunction (ED) is a condition in which an individual has difficulty either initiating or maintaining an erection of the clitoris or penis. The combined prevalence of minimal, moderate, and complete ED is approximately 40 percent at age 40, and reaches nearly 70 percent by 70 years of age. In addition to aging, ED is associated with diabetes, vascular disease, psychiatric disorders, prostate disorders, and the use of some drugs such as certain antidepressants. These physical and emotional conditions can lead to interruptions in the vasodilation pathway and result in an inability to achieve an erection of the penis or clitoris.
Recall that the release of NO induces relaxation of the smooth muscles that surround the erectile tissue arteries, leading to the vasodilation necessary to achieve an erection of the clitoris or penis. To reverse the process of vasodilation, an enzyme called phosphodiesterase (PDE) degrades a key component of the NO signaling pathway called cGMP. There are several different forms of this enzyme, and PDE type 5 is the type of PDE found in the tissues of the penis and clitoris. Scientists discovered that inhibiting PDE5 increases blood flow, and allows vasodilation to occur.
Chapter Review
The reproductive systems of males and females begin to develop soon after conception. A gene on the male’s Y chromosome called SRY is critical in stimulating a cascade of events that simultaneously stimulate testis development and repress the development of female structures. Testosterone produced by Leydig cells in the embryonic testis stimulates the development of male sexual organs. If testosterone is not present, female sexual organs will develop.
Whereas the gonads and some other reproductive tissues are considered bipotential, the tissue that forms the internal reproductive structures stems from ducts that will develop into only male (Wolffian) or female (Müllerian) structures. To be able to reproduce as an adult, one of these systems must develop properly and the other must degrade.
Further development of the reproductive systems occurs at puberty. The initiation of the changes that occur in puberty is the result of a decrease in sensitivity to negative feedback in the hypothalamus and pituitary gland, and an increase in sensitivity of the gonads to FSH and LH stimulation. These changes lead to increases in either estrogen or testosterone, in female and male adolescents, respectively. The increase in sex steroid hormones leads to maturation of the gonads and other reproductive organs. The initiation of spermatogenesis begins in boys, and girls begin ovulating and menstruating. Increases in sex steroid hormones also lead to the development of secondary sex characteristics such as breast development in girls and facial hair and larynx growth in boys.
Interactive Link Questions
A baby’s gender is determined at conception, and the different genitalia of male and female fetuses develop from the same tissues in the embryo. View this animation that compares the development of structures of the female and male reproductive systems in a growing fetus. Where are the testes located for most of gestational time?
The testes are located in the abdomen.
Review Questions
Critical Thinking Questions
1. Identify the changes in sensitivity that occur in the hypothalamus, pituitary, and gonads as a boy or girl approaches puberty. Explain how these changes lead to the increases of sex steroid hormone secretions that drive many pubertal changes.
2. Explain how the internal female and male reproductive structures develop from two different duct systems.
3. Explain what would occur during fetal development to an XY individual with a mutation causing a nonfunctional SRY gene.
Glossary
- Müllerian duct
- duct system present in the embryo that will eventually form the internal female reproductive structures
- puberty
- life stage during which a male or female adolescent becomes anatomically and physiologically capable of reproduction
- secondary sex characteristics
- physical characteristics that are influenced by sex steroid hormones and have supporting roles in reproductive function
- Wolffian duct
- duct system present in the embryo that will eventually form the internal male reproductive structures
Solutions
Answers for Critical Thinking Questions
- As an individual approaches puberty, two changes in sensitivity occur. The first is a decrease of sensitivity in the hypothalamus and pituitary to negative feedback, meaning that it takes increasingly larger concentrations of sex steroid hormones to stop the production of LH and FSH. The second change in sensitivity is an increase in the sensitivity of the gonads to the FSH and LH signals, meaning that the gonads of adults are more responsive to gonadotropins than are the gonads of children. As a result of these two changes, the levels of LH and FSH slowly increase and lead to the enlargement and maturation of the gonads, which in turn leads to secretion of higher levels of sex hormones and the initiation of spermatogenesis and folliculogenesis.
- The internal reproductive structures form from one of two rudimentary duct systems in the embryo. Testosterone secretion stimulates growth of the male tract, the Wolffian duct. Secretions of sustentacular cells trigger a degradation of the female tract, the Müllerian duct. Without these stimuli, the Müllerian duct will develop and the Wolffian duct will degrade, resulting in a female embryo.
- If the SRY gene were not functional, the XY individual would be genetically a male, but would develop female reproductive structures.
This work, Anatomy & Physiology, is adapted from Anatomy & Physiology by OpenStax, licensed under CC BY. This edition, with revised content and artwork, is licensed under CC BY-SA except where otherwise noted.
Images, from Anatomy & Physiology by OpenStax, are licensed under CC BY except where otherwise noted.
Access the original for free at https://openstax.org/books/anatomy-and-physiology/pages/1-introduction.

