20.3 Viral Infections of the Circulatory and Lymphatic Systems
Learning Objectives
- Identify common viral pathogens that cause infections of the circulatory and lymphatic systems
- Compare the major characteristics of specific viral diseases affecting the circulatory and lymphatic systems
Viral pathogens of the circulatory system vary tremendously both in their virulence and distribution worldwide. Some of these pathogens are practically global in their distribution. Fortunately, the most ubiquitous viruses tend to produce the mildest forms of disease. In the majority of cases, those infected remain asymptomatic. On the other hand, other viruses are associated with life-threatening diseases that have impacted human history.
Infectious Mononucleosis and Burkitt Lymphoma
Human herpesvirus 4, also known as Epstein-Barr virus (EBV), has been associated with a variety of human diseases, such as mononucleosis and Burkitt lymphoma. Exposure to the human herpesvirus 4 (HHV-4) is widespread and nearly all people have been exposed at some time in their childhood, as evidenced by serological tests on populations. The virus primarily resides within B lymphocytes and, like all herpes viruses, can remain dormant in a latent state for a long time.
When uninfected young adults are exposed to EBV, they may experience infectious mononucleosis. The virus is mainly spread through contact with body fluids (e.g., saliva, blood, and semen). The main symptoms include pharyngitis, fever, fatigue, and lymph node swelling. Abdominal pain may also occur as a result of spleen and liver enlargement in the second or third week of infection. The disease typically is self-limiting after about a month. The main symptom, extreme fatigue, can continue for several months, however. Complications in immunocompetent patients are rare but can include jaundice, anemia, and possible rupture of the spleen caused by enlargement.
In patients with malaria or HIV, Epstein-Barr virus can lead to a fast-growing malignant cancer known as Burkitt lymphoma. This condition is a form of non-Hodgkin lymphoma that produces solid tumors chiefly consisting of aberrant B cells. Burkitt lymphoma is more common in Africa, where prevalence of HIV and malaria is high, and it more frequently afflicts children.
Infectious mononucleosis is typically diagnosed based on the initial clinical symptoms and a test for antibodies to EBV-associated antigens. Because the disease is self-limiting, antiviral treatments are rare for mononucleosis. Cases of Burkitt lymphoma are diagnosed from a biopsy specimen from a lymph node or tissue from a suspected tumor.
Ebola Virus Disease
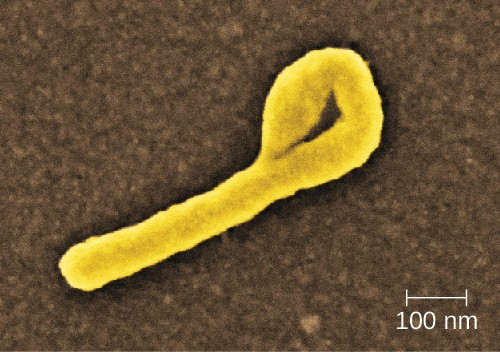
The Ebola virus disease (EVD) is a highly contagious disease caused by species of Ebolavirus, a BSL-4 filovirus (Figure 20.14). Transmission to humans occurs through direct contact with body fluids (e.g., blood, saliva, sweat, urine, feces, or vomit), and indirect contact by contaminated fomites. Infected patients can easily transmit Ebola virus to others if appropriate containment and use of personal protective equipment is not available or used. Handling and working with patients with EVD is extremely hazardous to the general population and health-care workers. In almost every EVD outbreak there have been Ebola infections among health-care workers. This ease of Ebola virus transmission was recently demonstrated in the Ebola epidemic in Guinea, Liberia, and Sierra Leone in 2014, in which more than 28,000 people in 10 countries were infected and more than 11,000 died.[1]
After infection, the initial symptoms of Ebola are unremarkable: fever, severe headache, myalgia, cough, chest pain, and pharyngitis. As the disease progresses, patients experience abdominal pain, diarrhea, and vomiting. Hemorrhaging begins after about 3 days, with bleeding occurring in the gastrointestinal tract, skin, and many other sites. This often leads to delirium, stupor, and coma, accompanied by shock, multiple organ failure, and death. The mortality rates of EVD often range from 50% to 90%.
The initial diagnosis of Ebola is difficult because the early symptoms are so similar to those of many other illnesses. It is possible to directly detect the virus from patient samples within a few days after symptoms begin, using antigen-capture ELISA, immunoglobulin M (IgM) ELISA, PCR, and virus isolation. There are currently no effective, approved treatments for Ebola other than supportive care and proper isolation techniques to contain its spread.
![]()
- How is Ebola transmitted?
Human Immunodeficiency Virus
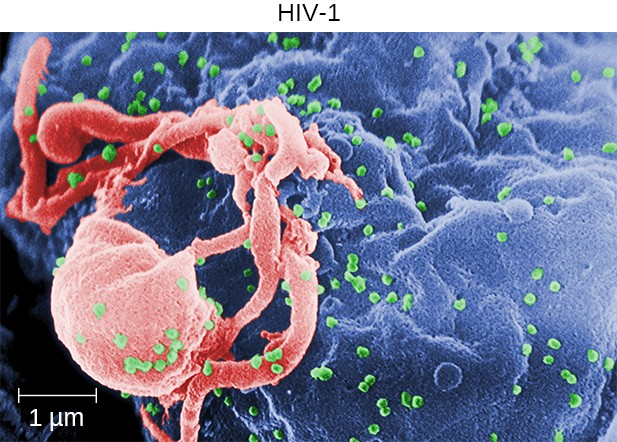
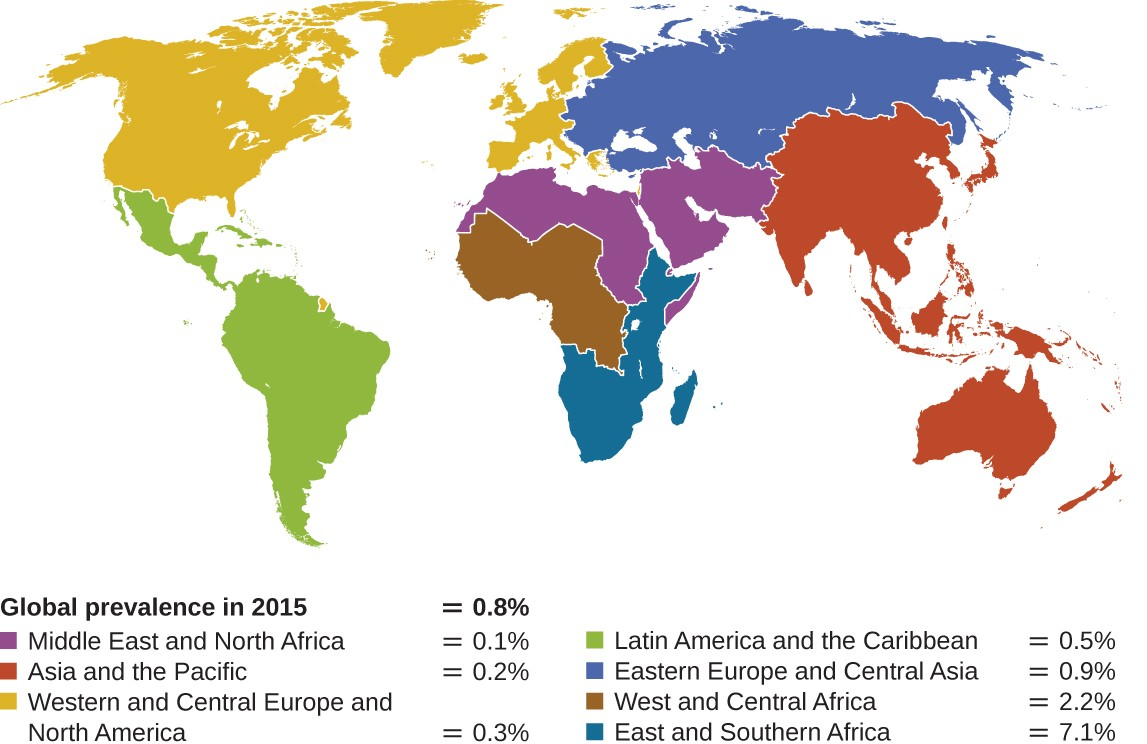
Human T-lymphotropic viruses (HTLV), also called human immunodeficiency viruses (HIV) are retroviruses that are the causative agent of acquired immune deficiency syndrome (AIDS). There are two main variants of human immunodeficiency virus (HIV). HIV-1 (Figure 20.15) occurs in human populations worldwide, whereas HIV-2 is concentrated in West Africa. Currently, the most affected region in the world is sub-Saharan Africa, with an estimated 25.6 million people living with HIV in 2015.[2] Sub-Saharan Africa also accounts for two-thirds of the global total of new HIV infections (Figure 20.16).[3]
HIV is spread through direct contact with body fluids. Casual contact and insect vectors are not sufficient for disease transmission; common modes of transmission include sexual contact and sharing of needles by intravenous (IV) drug users. It generally takes many years before the effects of an HIV infection are detected. HIV infections are not dormant during this period: virions are continually produced, and the immune system continually attempts to clear the viral infection, while the virus persistently infects additional CD4 T cells. Over time, the CD4 T-cell population is devastated, ultimately leading to AIDS.
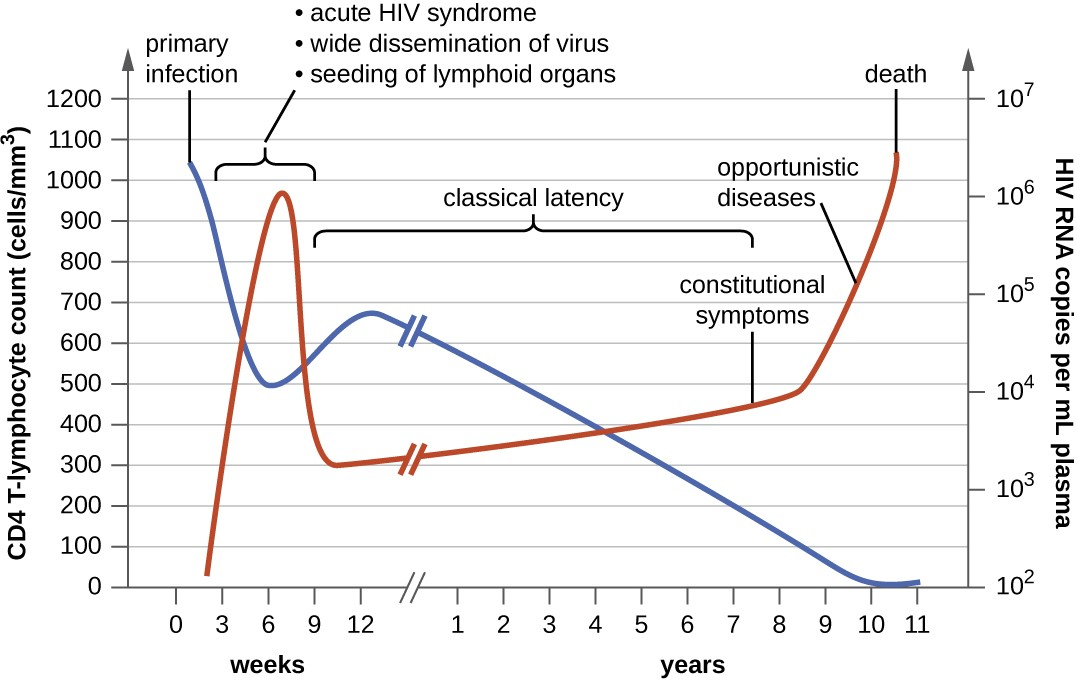
When people are infected with HIV, their disease progresses through three stages based on CD4 T-cell counts and the presence of clinical symptoms (Figure 20.17).
- Stage 1: Acute HIV infection. Two to 4 weeks after infection with HIV, patients may experience a flu- like illness, which can last for a few weeks. Patients with acute HIV infection have more than 500 cells/μL CD4 T cells and a large amount of virus in their blood. Patients are very contagious during this stage. To confirm acute infection, either a fourth-generation antibody-antigen test or a nucleic acid test (NAT) must be performed.
- Stage 2: Clinical latency. During this period, HIV enters a period of dormancy. Patients have between 200 and 499 cells/μL CD4 T cells; HIV is still active but reproduces at low levels, and patients may not experience any symptoms of illness. For patients who are not taking medicine to treat HIV, this period can last a decade or longer. For patients receiving antiretroviral therapy, the stage may last for several decades, and those with low levels of the virus in their blood are much less likely to transmit HIV than those who are not virally suppressed. Near the end of the latent stage, the patient’s viral load starts to increase and the CD4 T-cell count begins to decrease, leading to the development of symptoms and increased susceptibility to opportunistic infections.
- Stage 3: Acquired immunodeficiency syndrome (AIDS). Patients are diagnosed with AIDS when their CD4 T-cell count drops below 200 cells/μL or when they develop certain opportunistic illnesses. During this stage, the immune system becomes severely damaged by HIV. Common symptoms of AIDS include chills, fever, sweats, swollen lymph glands, weakness, and weight loss; in addition, patients often develop rare cancers such as Kaposi’s sarcoma and opportunistic infections such as Pneumocystis pneumonia, tuberculosis, cryptosporidiosis, and toxoplasmosis. This is a fatal progression that, in the terminal stages, includes wasting syndrome and dementia complex. Patients with AIDS have a high viral load and are highly infectious; they typically survive about 3 years without treatment.
The initial diagnosis of HIV is performed using a serological test for antibody production against the pathogen. Positive test results are confirmed by Western blot or PCR tests. It can take weeks or months for the body to produce antibodies in response to an infection. There are fourth-generation tests that detect HIV antibodies and HIV antigens that are present even before the body begins producing antibodies. Nucleic acid tests (NATs) are a third type of test that is relatively expensive and uncommon; NAT can detect HIV in blood and determine the viral load.
As a consequence of provirus formation, it is currently not possible to eliminate HIV from an infected patient’s body. Elimination by specific antibodies is ineffective because the virus mutates rapidly—a result of the error-prone reverse transcriptase and the inability to correct errors. Antiviral treatments, however, can greatly extend life expectancy. To combat the problem of drug resistance, combinations of antiretroviral drugs called antiretroviral therapy (ART), sometimes called highly active ART or combined ART, are used. There are several different targets for antiviral drug action (and a growing list of drugs for each of these targets). One class of drugs inhibits HIV entry; other classes inhibit reverse transcriptase by blocking viral RNA-dependent and DNA-dependent DNA polymerase activity; and still others inhibit one of the three HIV enzymes needed to replicate inside human cells.
![]()
- Why is it not yet possible to cure HIV infections?
| Disease | Pathogen | Signs and Symptoms | Transmission | Diagnostic Tests | Antimicrobial Drugs |
|---|---|---|---|---|---|
| AIDS/HIV infection | Human immunodeficiency virus (HIV) | Flu-like symptoms during acute stage, followed by long period of clinical latency; final stage (AIDS) includes fever, weight loss, wasting syndrome, dementia, and opportunistic secondary infections leading to death | Contact with body fluids (e.g., sexual contact, use of contaminated needles) | Serological tests for antibodies and/or HIV antigens; nucleic acid test (NAT) for presence of virus | Antiretroviral therapy (ART) using various combinations of drugs |
| Burkitt lymphoma | Epstein-barr virus (human herpesvirus-4 [HHV-4]) | Rapid formation of malignant B-cell tumors, oral hairy leukoplakia; fatal if not promptly treated | Contact with body fluids (e.g., saliva, blood, semen); primarily affects patients immune-compromised by HIV or malaria | CT scans, tumor biopsy | Intensive alternating chemotherapy regimen |
| Ebola virus disease (EVD) | Ebola virus | Fever, headache, joint pain, diarrhea, vomiting, hemorrhaging in gastrointestinal tract, organ failure; often fatal | Contact with body fluids (e.g., blood, saliva, sweat, urine, feces, vomit); highly contagious | ELISA, IgM ELISA, PCR, virus isolation | None |
| Infectious mononucleosis | Epstein-Barr Virus (HHV-4), cytomegalovirus (HHV-5) | Pharyngitis, fever, extreme fatigue; swelling of lymph nodes, spleen, and liver | Contact with body fluids (e.g., saliva, blood, semen) | Tests for antibodies to various EBV-associated antigens | None |

