16.2 Bacterial Infections of the Skin and Eyes
Learning Objectives
- Identify the most common bacterial pathogens that cause infections of the skin and eyes
- Compare the major characteristics of specific bacterial diseases affecting the skin and eyes
Despite the skin’s protective functions, infections are common. Gram-positive Staphylococcus spp. and Streptococcus spp. are responsible for many of the most common skin infections. However, many skin conditions are not strictly associated with a single pathogen. Opportunistic pathogens of many types may infect skin wounds, and individual cases with identical symptoms may result from different pathogens or combinations of pathogens.
In this section, we will examine some of the most important bacterial infections of the skin and eyes and discuss how biofilms can contribute to and exacerbate such infections. Key features of bacterial skin and eye infections are also summarized in the Disease Profile boxes throughout this section.
Staphylococcal Infections of the Skin
Staphylococcus species are commonly found on the skin, with S. epidermidis and S. hominis being prevalent in the normal microbiota. S. aureus is also commonly found in the nasal passages and on healthy skin, but pathogenic strains are often the cause of a broad range of infections of the skin and other body systems.
S. aureus is quite contagious. It is spread easily through skin-to-skin contact, and because many people are chronic nasal carriers (asymptomatic individuals who carry S. aureus in their nares), the bacteria can easily be transferred from the nose to the hands and then to fomites or other individuals. Because it is so contagious, S. aureus is prevalent in most community settings. This prevalence is particularly problematic in hospitals, where antibiotic- resistant strains of the bacteria may be present, and where immunocompromised patients may be more susceptible to infection. Resistant strains include methicillin-resistant S. aureus (MRSA), which can be acquired through health- care settings (hospital-acquired MRSA, or HA-MRSA) or in the community (community-acquired MRSA, or CA- MRSA). Hospital patients often arrive at health-care facilities already colonized with antibiotic-resistant strains of S. aureus that can be transferred to health-care providers and other patients. Some hospitals have attempted to detect these individuals in order to institute prophylactic measures, but they have had mixed success (see Eye on Ethics: Screening Patients for MRSA).
When a staphylococcal infection develops, choice of medication is important. As discussed above, many staphylococci (such as MRSA) are resistant to some or many antibiotics. Thus, antibiotic sensitivity is measured to identify the most suitable antibiotic. However, even before receiving the results of sensitivity analysis, suspected S. aureus infections are often initially treated with drugs known to be effective against MRSA, such as trimethoprim- sulfamethoxazole (TMP/SMZ), clindamycin, a tetracycline (doxycycline or minocycline), or linezolid.
The pathogenicity of staphylococcal infections is often enhanced by characteristic chemicals secreted by some strains. Staphylococcal virulence factors include hemolysins called staphylolysins, which are cytotoxic for many types of cells, including skin cells and white blood cells. Virulent strains of S. aureus are also coagulase-positive, meaning they produce coagulase, a plasma-clotting protein that is involved in abscess formation. They may also produce leukocidins, which kill white blood cells and can contribute to the production of pus and Protein A, which inhibits phagocytosis by binding to the constant region of antibodies. Some virulent strains of S. aureus also produce other toxins, such as toxic shock syndrome toxin-1 (see Virulence Factors of Bacterial and Viral Pathogens).
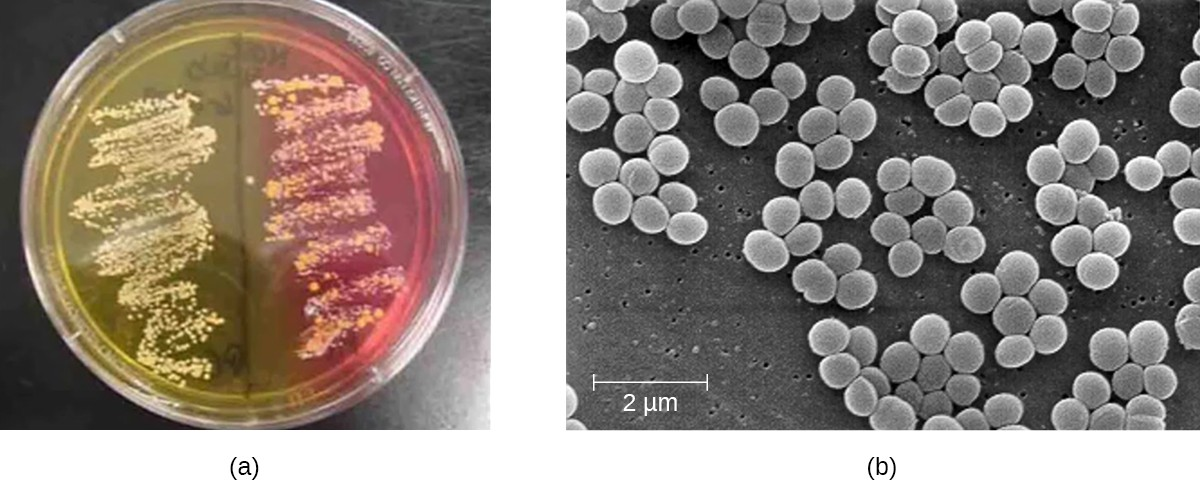
To confirm the causative agent of a suspected staphylococcal skin infection, samples from the wound are cultured. Under the microscope, gram-positive Staphylococcus species have cellular arrangements that form grapelike clusters; when grown on blood agar, colonies have a unique pigmentation ranging from opaque white to cream. A catalase test is used to distinguish Staphylococcus from Streptococcus, which is also a genus of gram-positive cocci and a common cause of skin infections. Staphylococcus species are catalase-positive while Streptococcus species are catalase-negative.
Other tests are performed on samples from the wound in order to distinguish coagulase-positive species of Staphylococcus (CoPS) such as S. aureus from common coagulase-negative species (CoNS) such as S. epidermidis. Although CoNS are less likely than CoPS to cause human disease, they can cause infections when they enter the body, as can sometimes occur via catheters, indwelling medical devices, and wounds. Passive agglutination testing can be used to distinguish CoPS from CoNS. If the sample is coagulase-positive, the sample is generally presumed to contain S. aureus. Additional genetic testing would be necessary to identify the particular strain of S. aureus.
Another way to distinguish CoPS from CoNS is by culturing the sample on mannitol salt agar (MSA). Staphylococcus species readily grow on this medium because they are tolerant of the high concentration of sodium chloride (7.5% NaCl). However, CoPS such as S. aureus ferment mannitol (which will be evident on a MSA plate), whereas CoNS such as S. epidermidis do not ferment mannitol but can be distinguished by the fermentation of other sugars such as lactose, malonate, and raffinose (Figure 16.7).
Eye on Ethics
Screening Patients for MRSA
According to the CDC, 86% of invasive MRSA infections are associated in some way with healthcare, as opposed to being community-acquired. In hospitals and clinics, asymptomatic patients who harbor MRSA may spread the bacteria to individuals who are more susceptible to serious illness.
In an attempt to control the spread of MRSA, hospitals have tried screening patients for MRSA. If patients test positive following a nasal swab test, they can undergo decolonization using chlorhexidine washes or intranasal mupirocin. Some studies have reported substantial reductions in MRSA disease following implementation of these protocols, while others have not. This is partly because there is no standard protocol for these procedures. Several different MRSA identification tests may be used, some involving slower culturing techniques and others rapid testing. Other factors, such as the effectiveness of general hand-washing protocols, may also play a role in helping to prevent MRSA transmission. There are still other questions that need to be addressed: How frequently should patients be screened? Which individuals should be tested? From where on the body should samples be collected? Will increased resistance develop from the decolonization procedures?
Even if identification and decolonization procedures are perfected, ethical questions will remain. Should patients have the right to decline testing? Should a patient who tests positive for MRSA have the right to decline the decolonization procedure, and if so, should hospitals have the right to refuse treatment to the patient? How do we balance the individual’s right to receive care with the rights of other patients who could be exposed to disease as a result?
Superficial Staphylococcal Infections
S. aureus is often associated with pyoderma, skin infections that are purulent. Pus formation occurs because many strains of S. aureus produce leukocidins, which kill white blood cells. These purulent skin infections may initially manifest as folliculitis, but can lead to furuncles or deeper abscesses called carbuncles.
Folliculitis generally presents as bumps and pimples that may be itchy, red, and/or pus-filled. In some cases, folliculitis is self-limiting, but if it continues for more than a few days, worsens, or returns repeatedly, it may require medical treatment. Sweat, skin injuries, ingrown hairs, tight clothing, irritation from shaving, and skin conditions can all contribute to folliculitis. Avoidance of tight clothing and skin irritation can help to prevent infection, but topical antibiotics (and sometimes other treatments) may also help. Folliculitis can be identified by skin inspection; treatment is generally started without first culturing and identifying the causative agent.
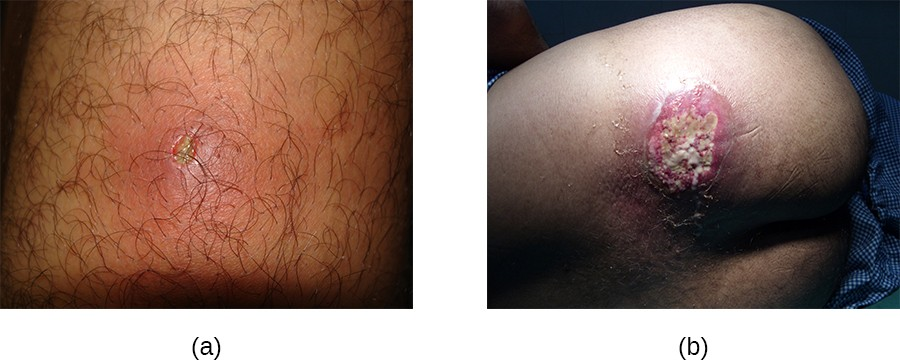
In contrast, furuncles (boils) are deeper infections (Figure 16.8). They are most common in those individuals (especially young adults and teenagers) who play contact sports, share athletic equipment, have poor nutrition, live in close quarters, or have weakened immune systems. Good hygiene and skin care can often help to prevent furuncles from becoming more infective, and they generally resolve on their own. However, if furuncles spread, increase in number or size, or lead to systemic symptoms such as fever and chills, then medical care is needed. They may sometimes need to be drained (at which time the pathogens can be cultured) and treated with antibiotics.
When multiple boils develop into a deeper lesion, it is called a carbuncle (Figure 16.8). Because carbuncles are deeper, they are more commonly associated with systemic symptoms and a general feeling of illness. Larger, recurrent, or worsening carbuncles require medical treatment, as do those associated with signs of illness such as fever. Carbuncles generally need to be drained and treated with antibiotics. While carbuncles are relatively easy to identify visually, culturing and laboratory analysis of the wound may be recommended for some infections because antibiotic resistance is relatively common.
Proper hygiene is important to prevent these types of skin infections or to prevent the progression of existing infections.
Staphylococcal scalded skin syndrome (SSSS) is another superficial infection caused by S. aureus that is most commonly seen in young children, especially infants. Bacterial exotoxins first produce erythema (redness of the skin) and then severe peeling of the skin, as might occur after scalding (Figure 16.9). SSSS is diagnosed by examining characteristics of the skin (which may rub off easily), using blood tests to check for elevated white blood cell counts, culturing, and other methods. Intravenous antibiotics and fluid therapy are used as treatment.

Impetigo
The skin infection impetigo causes the formation of vesicles, pustules, and possibly bullae, often around the nose and mouth. Bullae are large, fluid-filled blisters that measure at least 5 mm in diameter. Impetigo can be diagnosed as either nonbullous or bullous. In nonbullous impetigo, vesicles and pustules rupture and become encrusted sores. Typically the crust is yellowish, often with exudate draining from the base of the lesion. In bullous impetigo, the bullae fill and rupture, resulting in larger, draining, encrusted lesions (Figure 16.10).
Especially common in children, impetigo is particularly concerning because it is highly contagious. Impetigo can be caused by S. aureus alone, by Streptococcus pyogenes alone, or by coinfection of S. aureus and S. pyogenes. Impetigo is often diagnosed through observation of its characteristic appearance, although culture and susceptibility testing may also be used.
Topical or oral antibiotic treatment is typically effective in treating most cases of impetigo. However, cases caused by S. pyogenes can lead to serious sequelae (pathological conditions resulting from infection, disease, injury, therapy, or other trauma) such as acute glomerulonephritis (AGN), which is severe inflammation in the kidneys.

Nosocomial S. epidermidis Infections
Though not as virulent as S. aureus, the staphylococcus S. epidermidis can cause serious opportunistic infections. Such infections usually occur only in hospital settings. S. epidermidis is usually a harmless resident of the normal skin microbiota. However, health-care workers can inadvertently transfer S. epidermidis to medical devices that are inserted into the body, such as catheters, prostheses, and indwelling medical devices. Once it has bypassed the skin barrier, S. epidermidis can cause infections inside the body that can be difficult to treat. Like S. aureus, S. epidermidis is resistant to many antibiotics, and localized infections can become systemic if not treated quickly. To reduce the risk of nosocomial (hospital-acquired) S. epidermidis, health-care workers must follow strict procedures for handling and sterilizing medical devices before and during surgical procedures.
![]()
- Why are Staphylococcus aureus infections often purulent?
Streptococcal Infections of the Skin
Streptococcus are gram-positive cocci with a microscopic morphology that resembles chains of bacteria. Colonies are typically small (1–2 mm in diameter), translucent, entire edge, with a slightly raised elevation that can be either nonhemolytic, alpha-hemolytic, or beta-hemolytic when grown on blood agar (Figure 16.11). Additionally, they are facultative anaerobes that are catalase-negative.

The genus Streptococcus includes important pathogens that are categorized in serological Lancefield groups based on the distinguishing characteristics of their surface carbohydrates. The most clinically important streptococcal species in humans is S. pyogenes, also known as group A streptococcus (GAS). S. pyogenes produces a variety of extracellular enzymes, including streptolysins O and S, hyaluronidase, and streptokinase. These enzymes can aid in transmission and contribute to the inflammatory response.[1] S. pyogenes also produces a capsule and M protein, a streptococcal cell wall protein. These virulence factors help the bacteria to avoid phagocytosis while provoking a substantial immune response that contributes to symptoms associated with streptococcal infections.
S. pyogenes causes a wide variety of diseases not only in the skin, but in other organ systems as well. Examples of diseases elsewhere in the body include pharyngitis and scarlet fever.
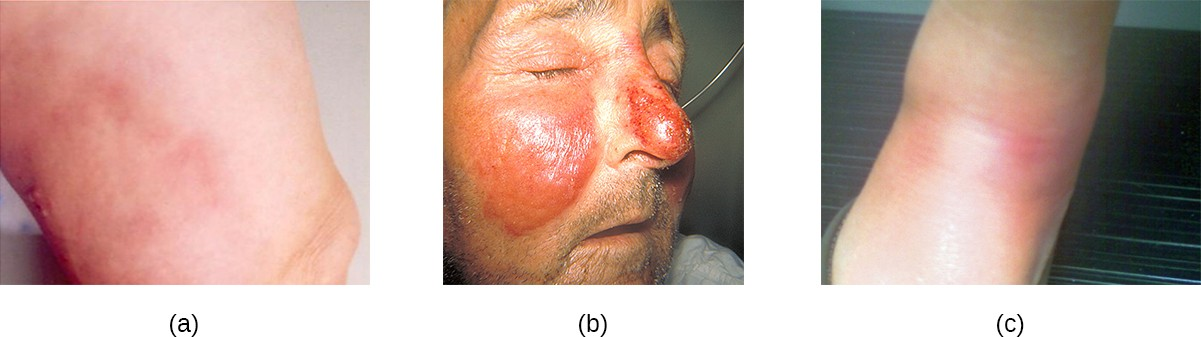
Cellulitis, Erysipelas, and Erythema Nosodum
Common streptococcal conditions of the skin include cellulitis and erysipelas. An infection that develops in the dermis or hypodermis can cause cellulitis, which presents as a reddened area of the skin that is warm to the touch and painful. The causative agent is often S. pyogenes, which may breach the epidermis through a cut or abrasion, although cellulitis may also be caused by staphylococci (Figure 16.12).
In general, streptococcal infections are best treated through identification of the specific pathogen followed by treatment based upon that particular pathogen’s susceptibility to different antibiotics. Many immunological tests, including agglutination reactions and ELISAs, can be used to detect streptococci. Penicillin is commonly prescribed for treatment of cellulitis and erysipelas because resistance is not widespread in streptococci at this time. Recommended treatments may include nonsteroidal anti-inflammatory drugs (NSAIDs), cool wet compresses, elevation, and bed rest.
Necrotizing Fasciitis
Streptococcal infections that start in the skin can sometimes spread elsewhere, resulting in a rare but potentially life-threatening condition called necrotizing fasciitis, sometimes referred to as flesh-eating bacterial syndrome. S. pyogenes is one of several species that can cause this rare but potentially-fatal condition; others include Klebsiella, Clostridium, Escherichia coli, S. aureus, and Aeromonas hydrophila.
Necrotizing fasciitis occurs when the fascia, a thin layer of connective tissue between the skin and muscle, becomes infected. Severe invasive necrotizing fasciitis due to Streptococcus pyogenes occurs when virulence factors that are responsible for adhesion and invasion overcome host defenses. S. pyogenes invasins allow bacterial cells to adhere to tissues and establish infection. Bacterial proteases unique to S. pyogenes aggressively infiltrate and destroy host tissues, inactivate complement, and prevent neutrophil migration to the site of infection. The infection and resulting tissue death can spread very rapidly, as large areas of skin become detached and die. Treatment generally requires debridement (surgical removal of dead or infected tissue) or amputation of infected limbs to stop the spread of the infection; surgical treatment is supplemented with intravenous antibiotics and other therapies (Figure 16.13).
Necrotizing fasciitis does not always originate from a skin infection; in some cases there is no known portal of entry.

![]()
- How do staphylococcal infections differ in general presentation from streptococcal infections?
Acne
One of the most ubiquitous skin conditions is acne. Acne afflicts nearly 80% of teenagers and young adults, but it can be found in individuals of all ages. Higher incidence among adolescents is due to hormonal changes that can result in overproduction of sebum.
Acne occurs when hair follicles become clogged by shed skin cells and sebum, causing non-inflammatory lesions called comedones. Comedones (singular “comedo”) can take the form of whitehead and blackhead pimples. Whiteheads are covered by skin, whereas blackhead pimples are not; the black color occurs when lipids in the clogged follicle become exposed to the air and oxidize (Figure 16.14).
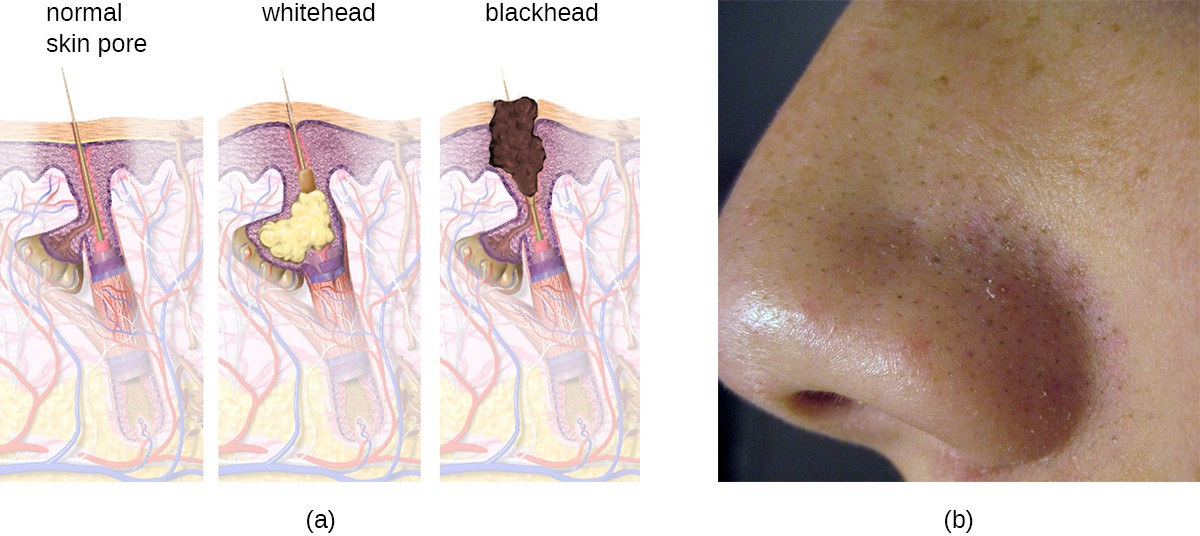
Often comedones lead to infection by Propionibacterium acnes, a gram-positive, non-spore-forming, aerotolerant anaerobic bacillus found on skin that consumes components of sebum. P. acnes secretes enzymes that damage the hair follicle, causing inflammatory lesions that may include papules, pustules, nodules, or pseudocysts, depending on their size and severity.
Treatment of acne depends on the severity of the case. There are multiple ways to grade acne severity, but three levels are usually considered based on the number of comedones, the number of inflammatory lesions, and the types of lesions. Mild acne is treated with topical agents that may include salicylic acid (which helps to remove old skin cells) or retinoids (which have multiple mechanisms, including the reduction of inflammation). Moderate acne may be treated with antibiotics (erythromycin, clindamycin), acne creams (e.g., benzoyl peroxide), and hormones. Severe acne may require treatment using strong medications such as isotretinoin (a retinoid that reduces oil buildup, among other effects, but that also has serious side effects such as photosensitivity). Other treatments, such as phototherapy and laser therapy to kill bacteria and possibly reduce oil production, are also sometimes used.
![]()
- What is the role of Propionibacterium acnes in causing acne?
Anthrax
The zoonotic disease anthrax is caused by Bacillus anthracis, a gram-positive, endospore-forming, facultative anaerobe. Anthrax mainly affects animals such as sheep, goats, cattle, and deer, but can be found in humans as well. Sometimes called wool sorter’s disease, it is often transmitted to humans through contact with infected animals or animal products, such as wool or hides. However, exposure to B. anthracis can occur by other means, as the endospores are widespread in soils and can survive for long periods of time, sometimes for hundreds of years.
The vast majority of anthrax cases (95–99%) occur when anthrax endospores enter the body through abrasions of the skin.[2] This form of the disease is called cutaneous anthrax. It is characterized by the formation of a nodule on the skin; the cells within the nodule die, forming a black eschar, a mass of dead skin tissue (Figure 16.15). The localized infection can eventually lead to bacteremia and septicemia. If untreated, cutaneous anthrax can cause death in 20% of patients.[3] Once in the skin tissues, B. anthracis endospores germinate and produce a capsule, which prevents the bacteria from being phagocytized, and two binary exotoxins that cause edema and tissue damage.

Less commonly, anthrax infections can be initiated through other portals of entry such as the digestive tract (gastrointestinal anthrax) or respiratory tract (pulmonary anthrax or inhalation anthrax). Typically, cases of noncutaneous anthrax are more difficult to treat than the cutaneous form. The mortality rate for gastrointestinal anthrax can be up to 40%, even with treatment. Inhalation anthrax, which occurs when anthrax spores are inhaled, initially causes influenza-like symptoms, but mortality rates are approximately 45% in treated individuals and 85% in those not treated. A relatively new form of the disease, injection anthrax, has been reported in Europe in intravenous drug users; it occurs when drugs are contaminated with B. anthracis. Patients with injection anthrax show signs and symptoms of severe soft tissue infection that differ clinically from cutaneous anthrax. This often delays diagnosis and treatment, and leads to a high mortality rate.[4]
B. anthracis colonies on blood agar have a rough texture and serrated edges that eventually form an undulating band (Figure 16.15). Broad spectrum antibiotics such as penicillin, erythromycin, and tetracycline are often effective treatments.
Unfortunately, B. anthracis has been used as a biological weapon and remains on the United Nations’ list of potential agents of bioterrorism.[5] Over a period of several months in 2001, a number of letters were mailed to members of the news media and the United States Congress. As a result, 11 individuals developed cutaneous anthrax and another 11 developed inhalation anthrax. Those infected included recipients of the letters, postal workers, and two other individuals. Five of those infected with pulmonary anthrax died. The anthrax spores had been carefully prepared to aerosolize, showing that the perpetrator had a high level of expertise in microbiology.[6]
A vaccine is available to protect individuals from anthrax. However, unlike most routine vaccines, the current anthrax vaccine is unique in both its formulation and the protocols dictating who receives it.[7] The vaccine is administered through five intramuscular injections over a period of 18 months, followed by annual boosters. The US Food and Drug Administration (FDA) has only approved administration of the vaccine prior to exposure for at-risk adults, such as individuals who work with anthrax in a laboratory, some individuals who handle animals or animal products (e.g., some veterinarians), and some members of the United States military. The vaccine protects against cutaneous and inhalation anthrax using cell-free filtrates of microaerophilic cultures of an avirulent, nonencapsulated strain of B. anthracis.[8] The FDA has not approved the vaccine for routine use after exposure to anthrax, but if there were ever an anthrax emergency in the United States, patients could be given anthrax vaccine after exposure to help prevent disease.
![]()
- What is the characteristic feature of a cutaneous anthrax infection?
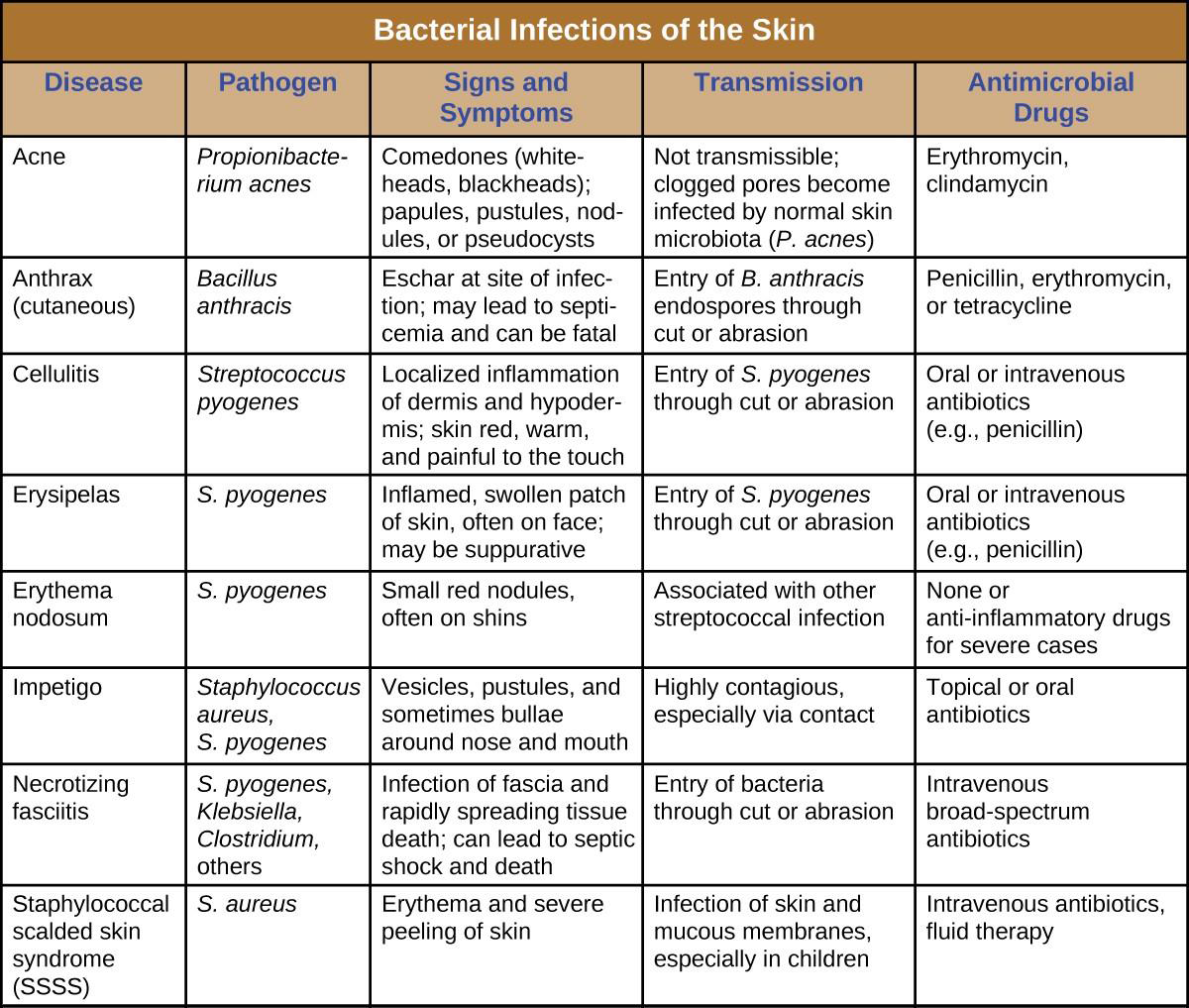
Disease Profile
Bacterial Infections of the Skin
Bacterial infections of the skin can cause a wide range of symptoms and syndromes, ranging from the superficial and relatively harmless to the severe and even fatal. Most bacterial skin infections can be diagnosed by culturing the bacteria and treated with antibiotics. Antimicrobial susceptibility testing is also often necessary because many strains of bacteria have developed antibiotic resistance. Figure 16.16 summarizes the characteristics of some common bacterial skin infections.
Bacterial Conjunctivitis
Like the skin, the surface of the eye comes in contact with the outside world and is somewhat prone to infection by bacteria in the environment. Bacterial conjunctivitis (pinkeye) is a condition characterized by inflammation of the conjunctiva, often accompanied by a discharge of sticky fluid (described as acute purulent conjunctivitis) (Figure 16.17). Conjunctivitis can affect one eye or both, and it usually does not affect vision permanently. Bacterial conjunctivitis is most commonly caused by Haemophilus influenzae, but can also be caused by other species such as Moraxella catarrhalis, S. pneumoniae, and S. aureus. The causative agent may be identified using bacterial cultures, Gram stain, and diagnostic biochemical, antigenic, or nucleic acid profile tests of the isolated pathogen. Bacterial conjunctivitis is very contagious, being transmitted via secretions from infected individuals, but it is also self-limiting.
Bacterial conjunctivitis usually resolves in a few days, but topical antibiotics are sometimes prescribed. Because this condition is so contagious, medical attention is recommended whenever it is suspected. Individuals who use contact lenses should discontinue their use when conjunctivitis is suspected. Certain symptoms, such as blurred vision, eye pain, and light sensitivity, can be associated with serious conditions and require medical attention.

![]()
- How are the bacteria that cause conjunctivitis acquired?
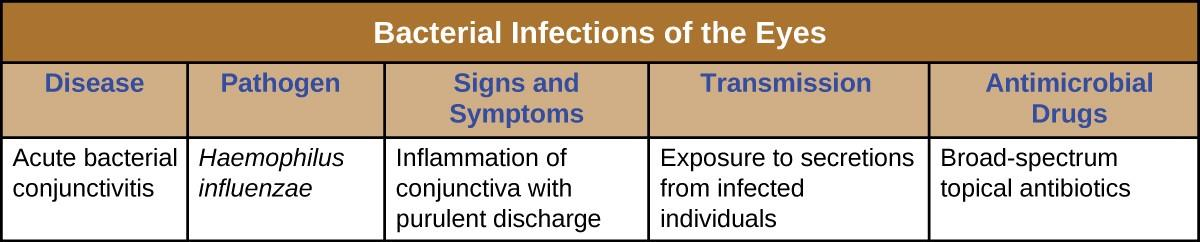
Disease Profile
Bacterial Infections of the Eyes
A number of bacteria are able to cause infection when introduced to the mucosa of the eye. In general, bacterial eye infections can lead to inflammation, irritation, and discharge, but they vary in severity. Some are typically short-lived, and others can become chronic and lead to permanent eye damage. Prevention requires limiting exposure to contagious pathogens. When infections do occur, prompt treatment with antibiotics can often limit or prevent permanent damage. Figure 16.18 summarizes the characteristics of some common bacterial infections of the eyes.
- Starr, C.R. and Engelberg N.C. “Role of Hyaluronidase in Subcutaneous Spread and Growth of Group A Streptococcus.” Infection and Immunity 2006(7:1): 40–48. doi: 10.1128/IAI.74.1.40-48.2006. ↵
- Shadomy, S.V., Traxler, R.M., and Marston, C.K. “Infectious Diseases Related to Travel: Anthrax” 2015. Centers for Disease Control and Prevention. http://wwwnc.cdc.gov/travel/yellowbook/2016/infectious-diseases-related-to-travel/anthrax. Accessed Sept 14, 2016. ↵
- US FDA. “Anthrax.” 2015. http://www.fda.gov/BiologicsBloodVaccines/Vaccines/ucm061751.htm. Accessed Sept 14, 2016. ↵
- Berger, T., Kassirer, M., and Aran, A.A.. “Injectional Anthrax—New Presentation of an Old Disease.” Euro Surveillance 19 (2014) 32. http://www.ncbi.nlm.nih.gov/pubmed/25139073. Accessed Sept 14, 2016. ↵
- United Nations Office at Geneva. “What Are Biological and Toxin Weapons?” http://www.unog.ch/80256EE600585943/%28httpPages%29/29B727532FECBE96C12571860035A6DB?. Accessed Sept 14, 2016. ↵
- Federal Bureau of Investigation. “Famous Cases and Criminals: Amerithrax or Anthrax Investigation.” https://www.fbi.gov/history/famous-cases/amerithrax-or-anthrax-investigation. Accessed Sept 14, 2016. ↵
- Centers for Disease Control and Prevention. “Anthrax: Medical Care: Prevention: Antibiotics.” http://www.cdc.gov/anthrax/medical-care/prevention.html. Accessed Sept 14, 2016. ↵
- Emergent Biosolutions. AVA (BioThrax) vaccine package insert (Draft). Nov 2015. http://www.fda.gov/downloads/biologicsbloodvaccines/bloodbloodproducts/approvedproducts/licensedproductsblas/ucm074923.pdf. ↵

