16.5 Helminthic Infections of the Skin and Eyes
Learning Objectives
- Identify two parasites that commonly cause infections of the skin and eyes
- Identify the major characteristics of specific parasitic diseases affecting the skin and eyes
Many parasitic protozoans and helminths use the skin or eyes as a portal of entry. Some may physically burrow into the skin or the mucosa of the eye; others breach the skin barrier by means of an insect bite. Still others take advantage of a wound to bypass the skin barrier and enter the body, much like other opportunistic pathogens. Although many parasites enter the body through the skin, in this chapter we will limit our discussion to those for which the skin or eyes are the primary site of infection. Parasites that enter through the skin but travel to a different site of infection will be covered in other chapters. In addition, we will limit our discussion to microscopic parasitic infections of the skin and eyes. Macroscopic parasites such as lice, scabies, mites, and ticks are beyond the scope of this text.
Loiasis
The helminth Loa loa, also known as the African eye worm, is a nematode that can cause loiasis, a disease endemic to West and Central Africa. The disease does not occur outside that region except when carried by travelers. There is evidence that individual genetic differences affect susceptibility to developing loiasis after infection by the Loa loa worm. Even in areas in which Loa loa worms are common, the disease is generally found in less than 30% of the population.[1] It has been suggested that travelers who spend time in the region may be somewhat more susceptible to developing symptoms than the native population, and the presentation of infection may differ.[2]
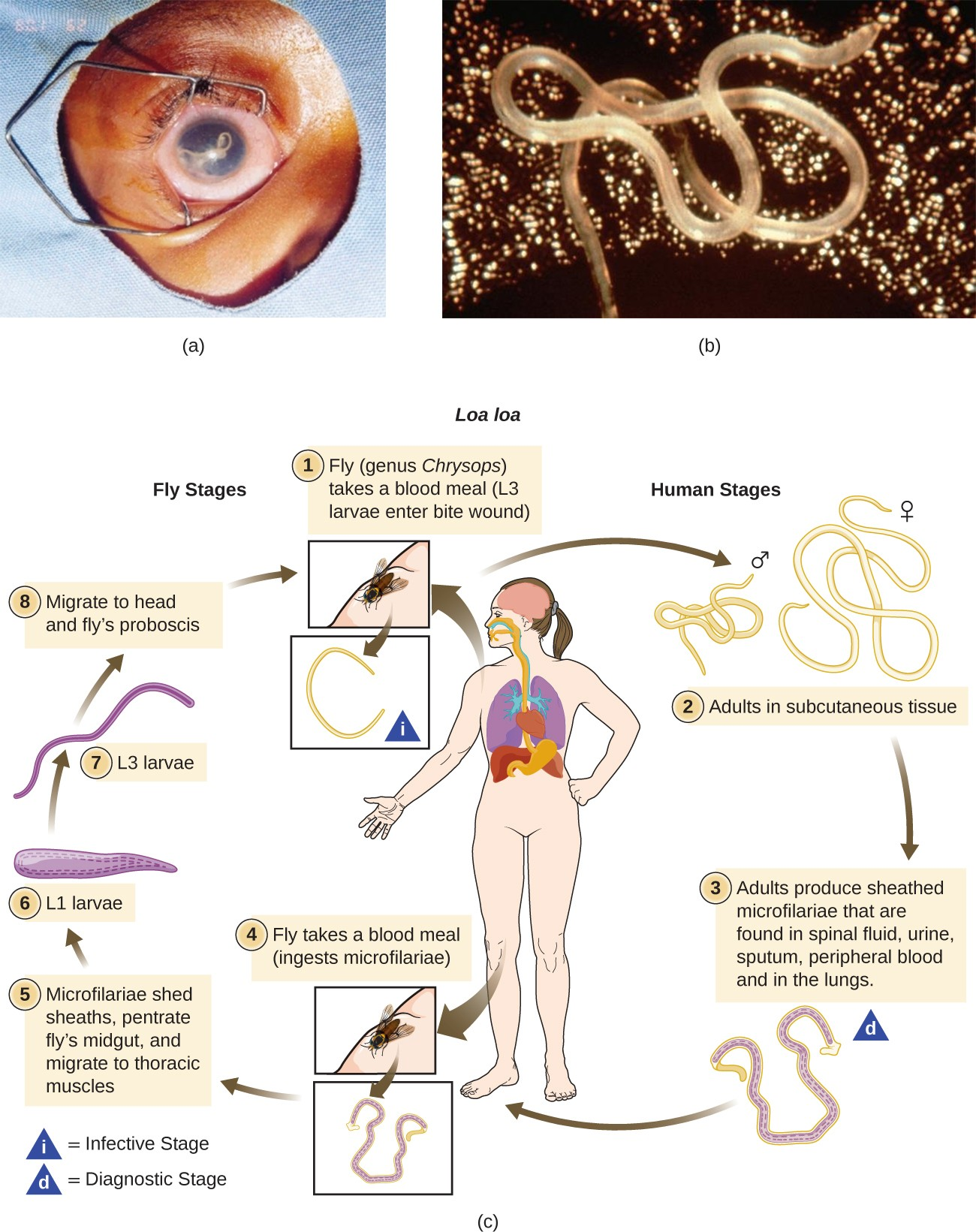
The parasite is spread by deerflies (genus Chrysops), which can ingest the larvae from an infected human via a blood meal (Figure 16.24). When the deerfly bites other humans, it deposits the larvae into their bloodstreams. After about five months in the human body, some larvae develop into adult worms, which can grow to several centimeters in length and live for years in the subcutaneous tissue of the host.
The name “eye worm” alludes to the visible migration of worms across the conjunctiva of the eye. Adult worms live in the subcutaneous tissues and can travel at about 1 cm per hour. They can often be observed when migrating through the eye, and sometimes under the skin; in fact, this is generally how the disease is diagnosed. It is also possible to test for antibodies, but the presence of antibodies does not necessarily indicate a current infection; it only means that the individual was exposed at some time. Some patients are asymptomatic, but in others the migrating worms can cause fever and areas of allergic inflammation known as Calabar swellings. Worms migrating through the conjunctiva can cause temporary eye pain and itching, but generally there is no lasting damage to the eye. Some patients experience a range of other symptoms, such as widespread itching, hives, and joint and muscle pain.
Worms can be surgically removed from the eye or the skin, but this treatment only relieves discomfort; it does not cure the infection, which involves many worms. The preferred treatment is diethylcarbamazine, but this medication produces severe side effects in some individuals, such as brain inflammation and possible death in patients with heavy infections. Albendazole is also sometimes used if diethylcarbamazine is not appropriate or not successful. If left untreated for many years, loiasis can damage the kidneys, heart, and lungs, though these symptoms are rare.
![]()
- Describe the most common way to diagnose loiasis.
Link to Learning
See a video (https://openstax.org/l/22microfilvid) of a live Loa loa microfilaria under the microscope.
Disease Profile
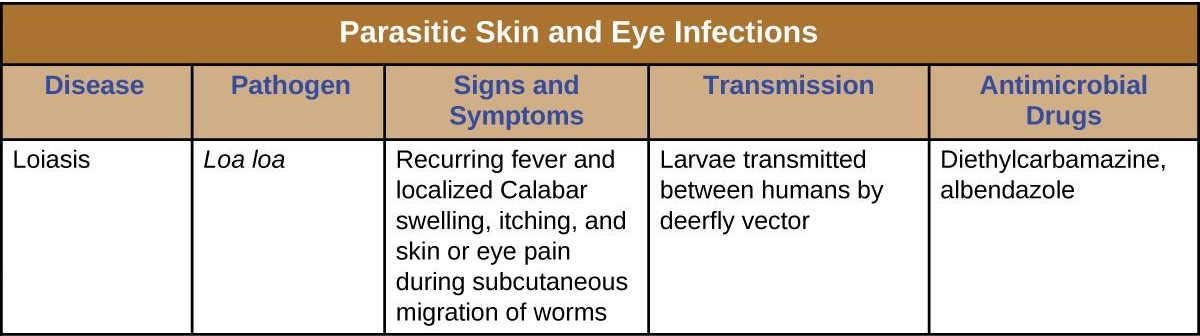
Parasitic Skin and Eye Infections
The protozoan Acanthamoeba and the helminth Loa loa are two parasites capable of causing infections of the skin and eyes. Figure 16.25 summarizes the characteristics of some common fungal infections of the skin.
- Garcia, A.. et al. “Genetic Epidemiology of Host Predisposition Microfilaraemia in Human Loiasis.” Tropical Medicine and International Health 4 (1999) 8:565–74. http://www.ncbi.nlm.nih.gov/pubmed/10499080. Accessed Sept 14, 2016. ↵
- Spinello, A., et al. “Imported Loa loa Filariasis: Three Cases and a Review of Cases Reported in Non-Endemic Countries in the Past 25 Years.” International Journal of Infectious Disease 16 (2012) 9: e649–e662. DOI: http://dx.doi.org/10.1016/j.ijid.2012.05.1023. ↵

